Neurol Neuroimmunol Neuroinflamm:糖尿病是抗自身抗体阳性的淋巴结病的危险因素
2022-05-14 从医路漫漫 MedSci原创
自身免疫的主要触发因素仍未确定。患者表现出独特的表型,经常表现为急性发作、严重感觉运动神经病、感觉性共济失调、震颤和神经性疼痛。
背景:在过去的十年里,淋巴结病已经成为周围神经病的一个新概念。在这种情况下,已经描述了针对细胞粘附分子的免疫球蛋白(Ig) G自身抗体,如接触蛋白-1、接触蛋白-1相关蛋白1 (Caspr-1)和神经筋膜蛋白亚型。这些蛋白在Ranvier结的结旁区域构成轴浆连接,对跳跃性传导至关重要。抗锥体抗体损害结的完整性和功能。然而,自身免疫的主要触发因素仍未确定。患者表现出独特的表型,经常表现为急性发作、严重感觉运动神经病、感觉性共济失调、震颤和神经性疼痛。IgG亚类可能会影响疾病的病程和对治疗的反应。因此,抗自身抗体是对监测和治疗有直接影响的新生物标志物。糖尿病性神经病变中也会出现Ranvier结处的轴索连接障碍,这可能使抗原暴露于免疫反应。糖尿病(DM)作为慢性炎性脱髓鞘性多发性神经根神经病(CIDP)的一个危险因素引起了争议,并在最近的多中心研究中得到证实。
目的:我们旨在研究抗体介导的淋巴结疾病和糖尿病(DM)之间的可能联系。
方法:我们回顾性分析了来自德国多个中心的227例慢性炎性脱髓鞘性多发性神经根神经病和格林-巴利综合征患者的临床资料,这些患者接受了针对神经束蛋白-155、泛神经束蛋白、接触蛋白-1相关蛋白1和接触蛋白-1的抗寄生虫抗体诊断试验。为了研究抗自身抗体可能的直接致病作用,我们对人胰腺组织切片进行了免疫荧光结合试验。
结果:血清阳性患者糖尿病患病率为33.3%,高于血清阴性患者(14.1%,OR = 3.04,95% CI = 1.31-6.80)。血清阳性患者患糖尿病的相对风险是德国普通人群的3.4倍。血清阳性的糖尿病患者最常携带抗接触蛋白-1抗体,且抗体滴度高于血清阳性的非糖尿病患者。在血清阳性患者中,糖尿病的诊断先于神经病变的发生。没有检测到针对胰腺组织的抗自身抗体的免疫反应性。
表1 队列的血清状态、诊断和人口统计学数据
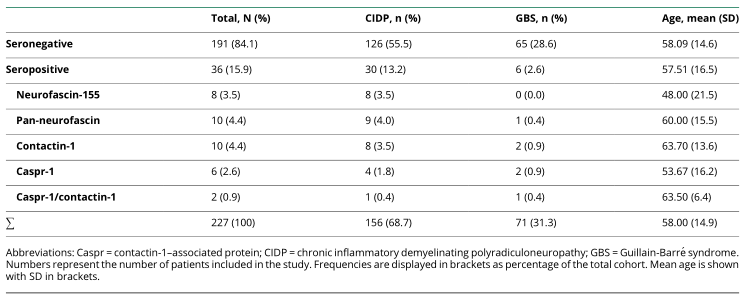
表2 统计测试结果
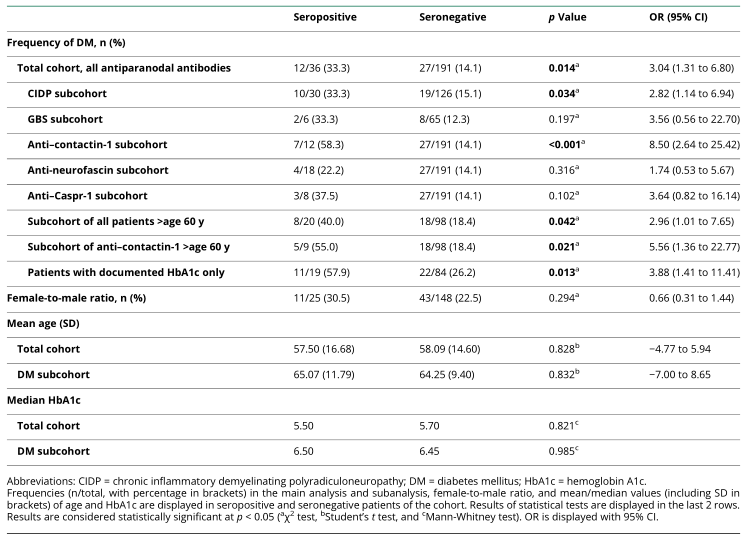

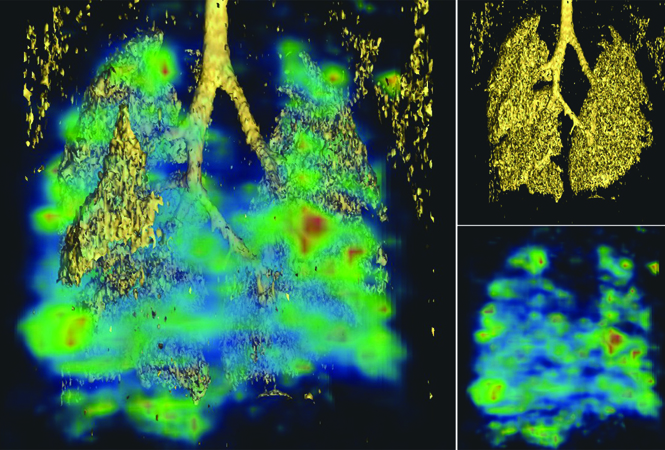
图 糖尿病的发生率和胰腺组织的免疫荧光染色。(A)与血清阴性患者(14.1%,p = 0.014)和德国普通人群(9.9%,p < 0.001)相比,抗自身抗体血清阳性患者(33.3%)患糖尿病的频率显著升高,尤其是在抗接触蛋白-1血清阳性患者中(58.3%对血清阴性患者的14.1%,p < 0.001)。在德国人口中分别为0.01%和9.9 %,p < 0.001)。显著性水平标有星号:*p < 0。0 5,* *p < 0.01,***p < 0.001。(B)在过去28天内未接受皮质类固醇治疗且首次接受利妥昔单抗治疗的血清阳性患者中,14名患者在抽血时测定了HbA1c水平(y轴,%), HbA1c水平与自身抗体滴度显著相关,以对数标度显示(r = 0)。5 8,p = 0.029)。(C.a–l)显微照片显示了人类胰腺正常组织切片,细胞核染色(DAPI)显示为蓝色(c . a、C.d、C.g和C.j ),突触素双重染色作为朗格汉斯胰岛(显示为绿色、C.b、C.e、C.h和C.k)和血清或抗自身抗体(显示为品红色、c . c . f、C.i和C.l)的标记。具有GAD抗体的CIDP和1型糖尿病患者的血清与胰岛β细胞结合(c . a–c ),而具有抗接触蛋白-1抗体(c . d–f)的患者的血清和商用山羊抗接触蛋白-1(c . g–I)和商用鸡抗泛神经束蛋白(c . j–l)不显示任何结合。未显示该试验中测试的其他患者血清或商品抗体结合的显微照片。比例尺= 10 μm CNTN = contact in-1;DAPI = 49,6-二脒基-2-苯基吲哚;DM =糖尿病;HbA1c =糖化血红蛋白。
结论:我们报道了淋巴结病和糖尿病的关系。我们的结果表明,糖尿病可能是易患淋巴结-副淋巴结病的潜在危险因素,并且糖尿病并非由自身抗体引起的。我们的发现为进一步研究潜在的免疫致病联系奠定了基础。
原文出处:Appeltshauser L, Messinger J, Starz K,et al.Diabetes Mellitus Is a Possible Risk Factor for Nodo-paranodopathy With Antiparanodal Autoantibodies.Neurol Neuroimmunol Neuroinflamm 2022 May;9(3)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#抗体阳性#
40
#LAM#
40
#Neurol#
0
学习了,了解到代谢性疾病的横纵向相关性
54
#淋巴结#
56
#NFL#
40