AAOS|三角韧带损伤的解剖、诊断与治疗
2022-05-25 骨科青年 网络
对于外踝骨折合并内踝三角韧带损伤患者,在固定外踝、稳定下胫腓后是否仍需固定三角韧带,仍存争议。

一、解剖与生物力学
距下关节类似于榫卯结构,内外后踝及其附属韧带结构、距骨穹隆、胫骨远端关节,共同构成距下关节。
内侧三角韧带起于内踝、止于距骨、跟骨及舟骨,三角韧带根据止点的不同分为深浅两层:
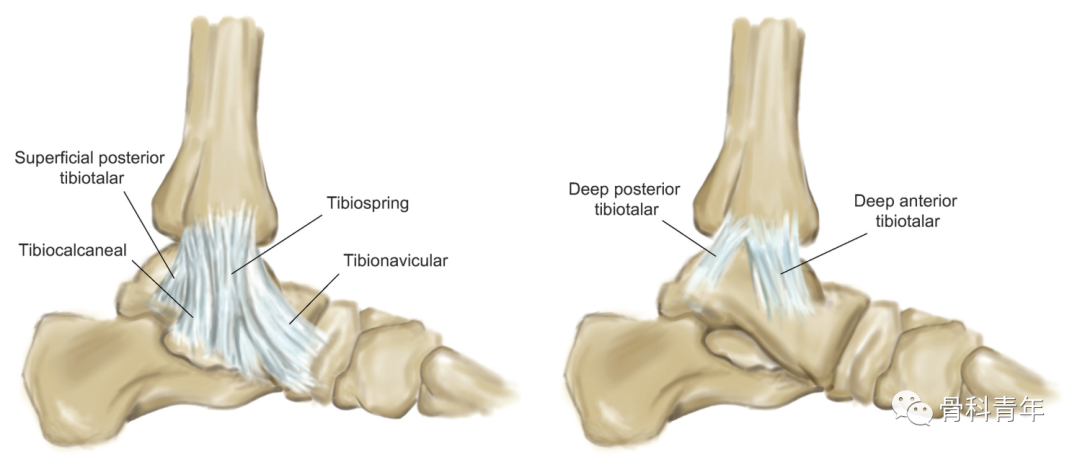
三角韧带对于踝关节的生物力学稳定至关重要。三角韧带的浅层能够限制后足的外翻,三角韧带的深层主要限制距骨外旋。
在一项尸体生物力学研究中,在旋后外旋的不同程度切断三角韧带或者进行内踝截骨,然后在轴向应力下活动踝关节,证实在旋后外旋I-III度损伤时距骨仍然可以维持正常的生理活动轨迹,只有在IV度损伤,即内踝三角韧带断裂时距骨活动轨迹才会变为异常。
1.手术顺序
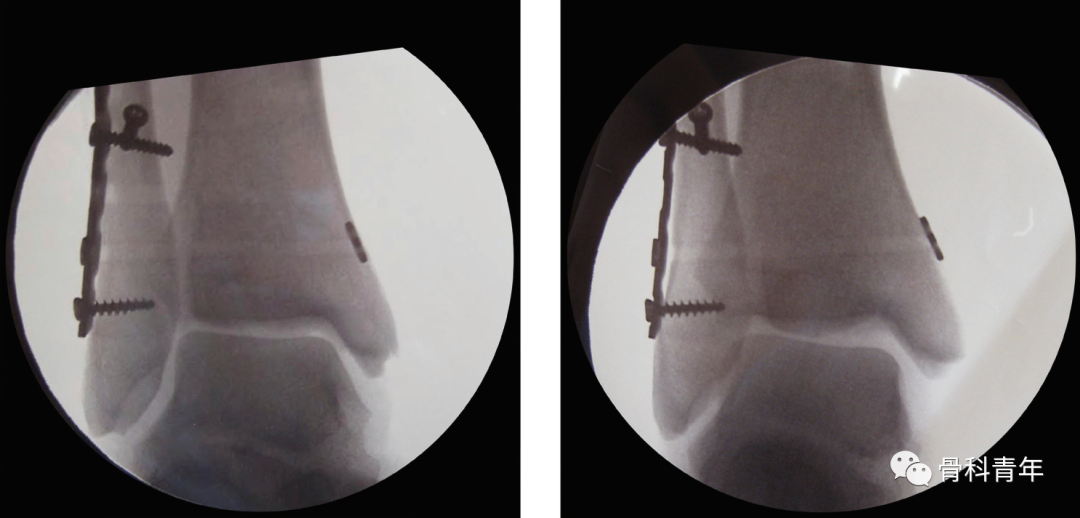
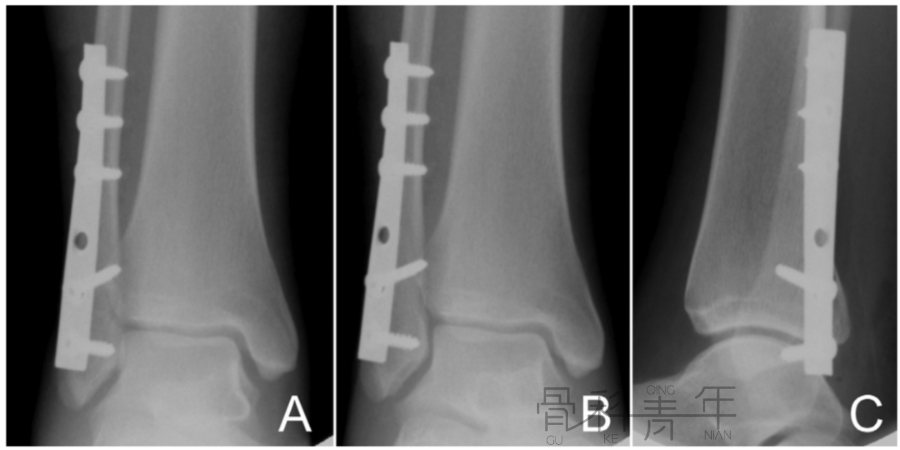
下胫腓稳定后需要进一步行应力位X线检查评估三角韧带情况,如果发现三角韧带损伤,建议进一步修复三角韧带。

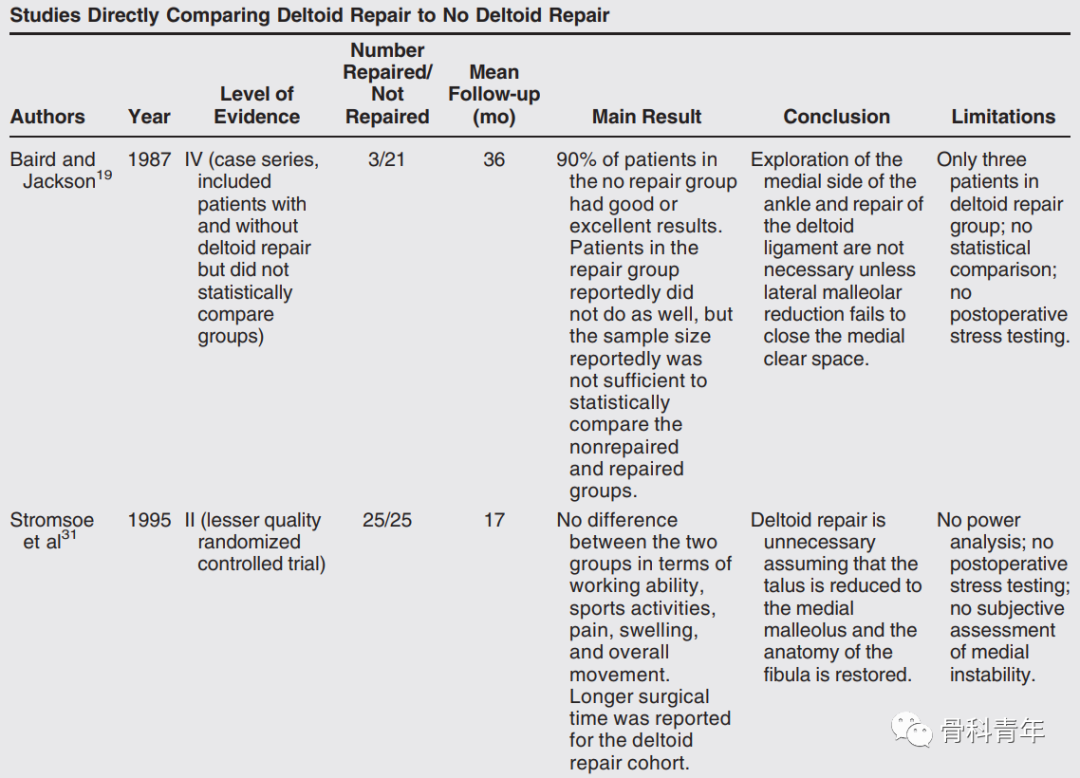
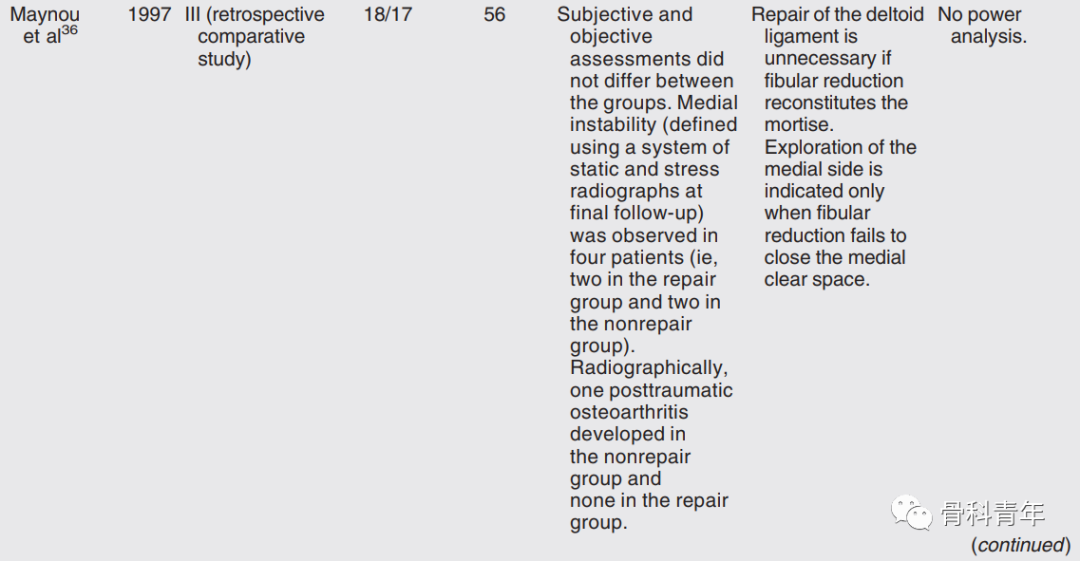
对于三角韧带损伤是否需要修复仍然存在争议。
有观点认为对于所有的三角韧带损伤都应该进行修复重建,因三角韧带未修复会导致骨折不稳定,需修复三角韧带以恢复内侧胫距稳定性。
而有观点认为只有在需要显露内侧间隙进行清理时才进行三角韧带修复,还有观点认为仅对于高强度运动员在关节镜证实三角韧带完全断裂的情况下才需要进行修复重建。有一部分学者认为应该根据术中固定骨折后外旋/距骨倾斜应力试验是决定是否行内踝三角韧带修复重建。有研究显示术中应力试验下距骨倾斜大于7度为三角韧带修复重建指征。
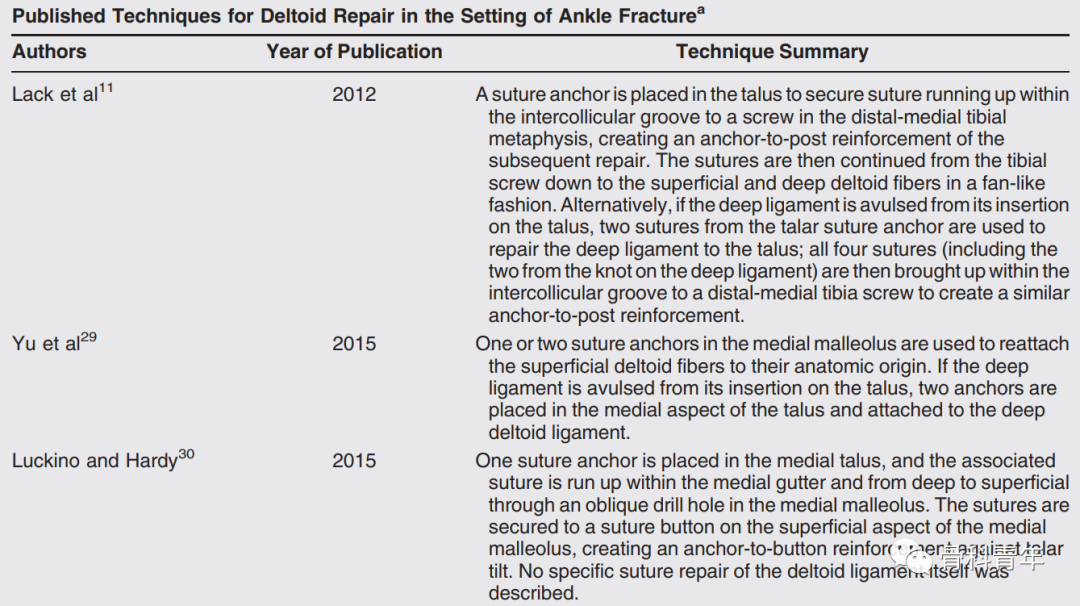
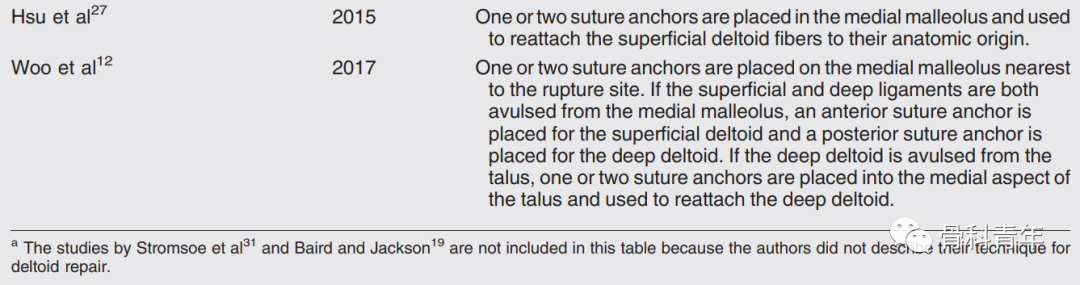
五、三角韧带重建
三角韧带的修补重建,文献中提出过诸多方法,但缺乏对各方法的比较研究。这些修补方法的共性在于以锚钉或缝线的方式,将三角韧带解剖重建于内踝。
推荐方法:
沿内踝中线取5cm弧形切口,牵开软组织可以显露三角韧带浅层、关节囊、胫后肌腱和三角韧带深层。通过向后下牵拉胫骨后肌腱,可以显露距骨软骨和内踝。
对于三角韧带内踝侧撕脱的病例(最常见),首先辨认并显露内踝尖,向近端剥离局部软组织1cm,制备锚钉钉道(下图左),可放置1-2枚带不可吸收缝合线的锚钉(下图右)。
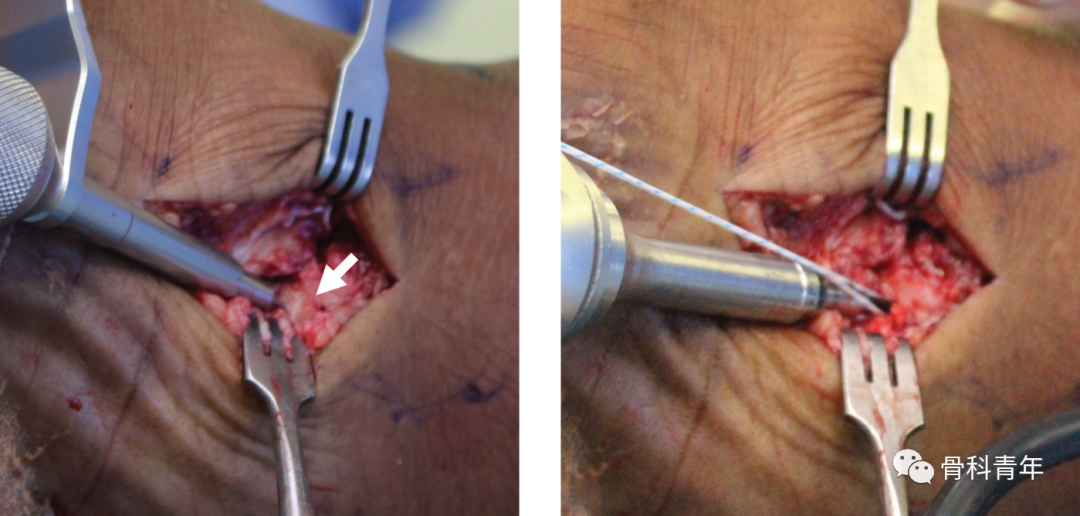
使用锚钉缝线叠瓦状缝合关节囊、三角韧带深层和浅层(下图),缝合后行外旋和外翻应力位测试三角韧带稳定性。
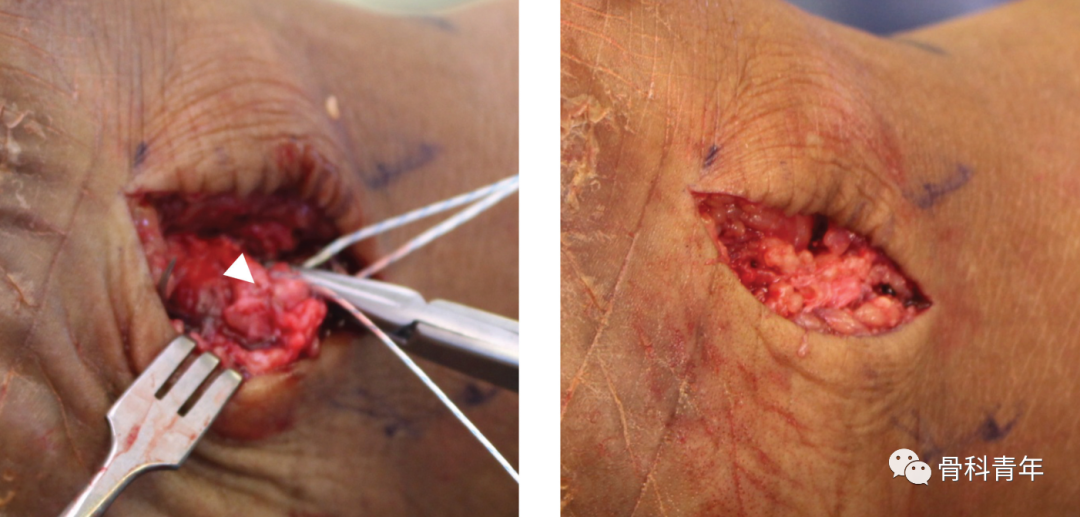
三角韧带远端撕脱情况较少,该损伤的修补方式,切口同内踝撕脱,注意保护胫骨后肌腱、胫后动脉和胫后神经。在距骨的内侧置入两枚锚钉,缝合三角韧带深浅层。
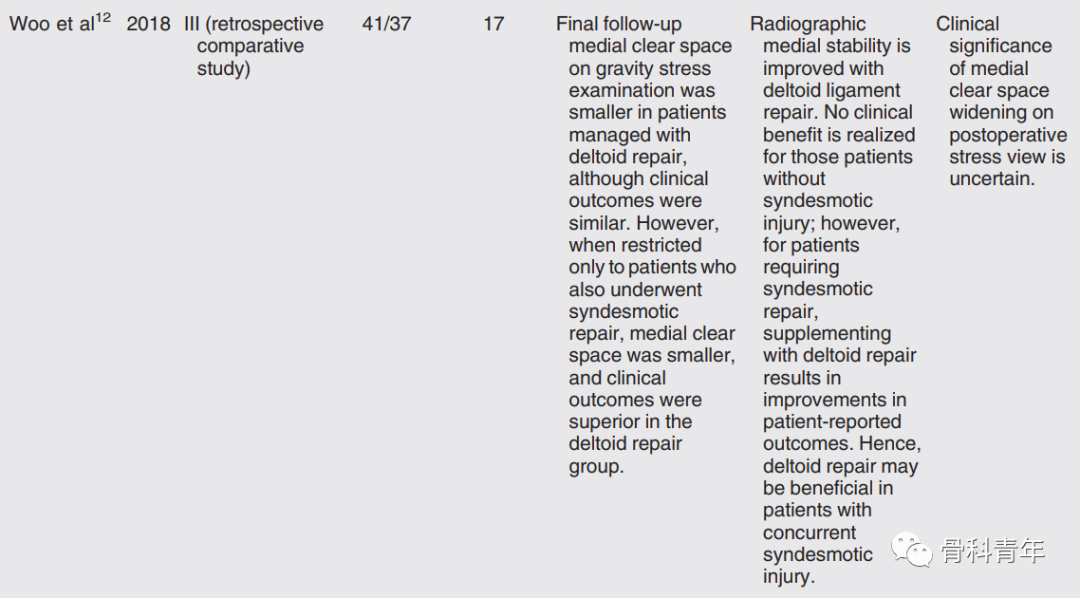
关于三角韧带修补的后功能结局,诸多文献研究提出了不同的结论,有兴趣者可搜索文献全文查看。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#AAO#
45
#诊断与治疗#
58
#AAOS#
47
学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习
51
#损伤#
49
#韧带#
46