Lenzilumab治疗COVID-19住院患者的III期临床:已取得阳性中期数据
2020-11-07 Allan MedSci原创
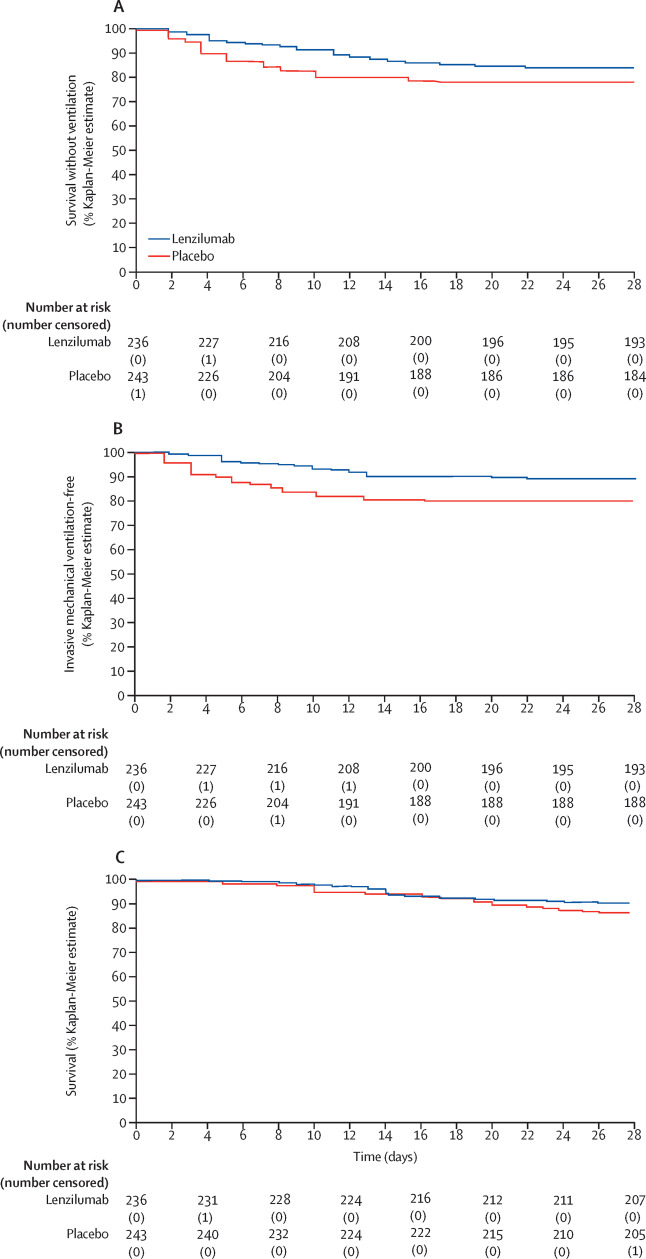
与目前的标准护理(SOC)相比,lenzilumab组中观察到的康复估计多了37%。
Humanigen是一家临床阶段的生物制药公司,致力于通过其领先的研究性疗法lenzilumab预防和治疗称为“细胞因子风暴”的过度免疫反应,Humanigen今天公布了积极的III期临床研究的中期数据。这项中期分析表明,lenzilumab对患者的康复具有临床意义,与目前的标准护理(SOC)相比,lenzilumab组中观察到的康复估计多了37%。

Humanigen首席执行官Cameron Durrant博士表示:“这些中期数据表明,lenzilumab有望成为COVID-19住院患者的一线治疗选择。这些数据以及lenzilumab对remdesivir和/或类固醇治疗的COVID-19患者可能产生的临床意义的影响令我们感到鼓舞”。
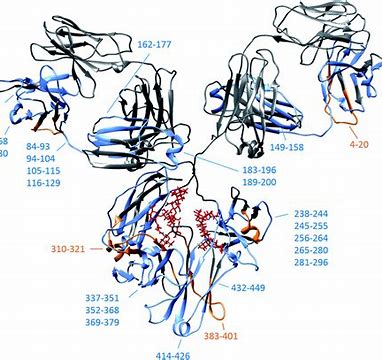
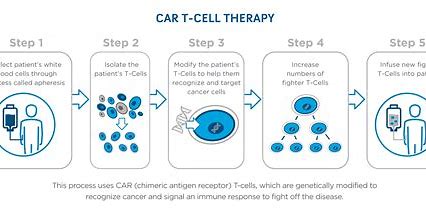
Lenzilumab是一种人源化单克隆抗体,靶向集落刺激因子2 /粒细胞-巨噬细胞集落刺激因子。临床前证据和临床数据提示,GM-CSF是全身炎症通路中的关键引发剂,该通路可导致严重且危及生命的嵌合抗原受体T细胞相关细胞激素释放综合征。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#I期临床#
36
#mAb#
30
#III#
36
#II期临床#
35
#III期#
37