Circ Arrhythm Electrophysiol:冠心病人运动不足或过度,猝死风险都增高!Circulation子刊研究称:每周2~3次理想
2020-05-25 朱朱 中国循环杂志
当前的美国稳定性缺血性心脏病患者诊断和管理指南建议,冠心病患者每周至少应有5天(最好每天)进行半小时至一小时的低中强度有氧运动,例如快走。
当前的美国稳定性缺血性心脏病患者诊断和管理指南建议,冠心病患者每周至少应有5天(最好每天)进行半小时至一小时的低中强度有氧运动,例如快走。
近日,一项研究提示,冠心病患者如果不经常运动,容易发生心原性猝死;对于有心绞痛症状的患者来说,运动过度时心原性猝死风险更高。
校正多个传统临床危险因素后的分析显示,平均随访6.3年期间,与每周坚持规律运动2~3次的患者相比,很少运动的冠心病患者出现心原性猝死的风险增加1.45倍,心原性死亡风险增加1.2倍。
研究者发现,在有症状即加拿大心血管学会心绞痛分级≥2级的患者中,与每周规律运动2~3次者相比,很少运动者发生心原性猝死的风险增加2.64倍,而运动过多(每周至少运动4次)者心原性猝死风险更高,增加6.46倍。
而对于没有心绞痛症状的冠心病患者来说,休闲时间运动与心原性猝死风险无关。
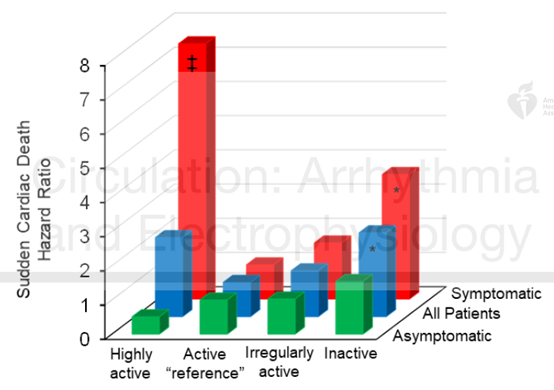
不同运动水平(纵向)以及有或无症状(横向)的冠心病患者的心原性猝死风险
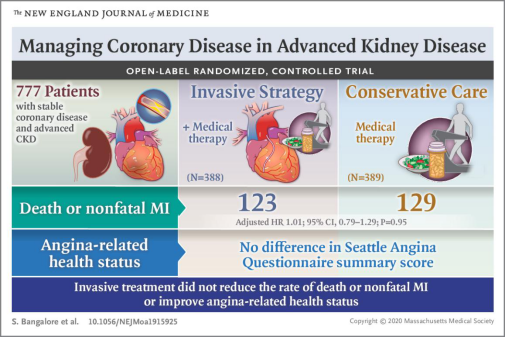
研究者指出,该研究表明,对于持续有明显心绞痛的冠心病患者来说,在频繁进行高强度运动训练前,需要进一步进行心肌缺血的功能性评估,且很可能需要加强治疗。
该研究还显示,休闲时间运动水平与非心原性猝死风险之前呈线性关系,运动最多的患者非心原性猝死风险最低,而且在有或无心绞痛症状的患者中均如此。
该研究纳入1946例经冠脉造影确诊的冠心病患者,其中1107例无症状。不经常运动的患者占11%,不规律运动者占36%,37%每周规律运动2~3次,16%每周规律运动至少4次。每周规律运动2~3次的患者中心原性猝死率最低,为1.5%。
原始出处:Mikko P Tulppo, Antti M Kiviniemi, Minna Lahtinen, et al. Physical Activity and the Risk for Sudden Cardiac Death in Patients with Coronary Artery Disease. Circulation: Arrhythmia and Electrophysiology, 20 May 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Physio#
39
#猝死风险#
44
#增高#
34
#增高#
34