Br J Cancer:TNIK抑制剂NCB-0846阻断TGFβ/SMAD信号通路抑制肺癌的转移
2020-12-08 xiaozeng MedSci原创
癌症的转移是癌症患者死亡的主要原因,目前仍是临床肿瘤学的一大主要挑战。上皮-间质转化(EMT)最初是在胚胎发育中提出的,越来越的的研究显示在癌症的转移过程中EMT起着至关重要的作用。
癌症的转移是癌症患者死亡的主要原因,目前仍是临床肿瘤学的一大主要挑战。上皮-间质转化(EMT)最初是在胚胎发育中提出的,越来越的的研究显示在癌症的转移过程中EMT起着至关重要的作用。
在EMT进程中,癌细胞失去上皮细胞的粘附/极性并获得间充质特性。EMT增加了细胞的可塑性和运动性,从而促进肿瘤细胞离开其原生部位,通过全身循环,并在远端重建肿瘤。因此,开发抑制EMT的治疗策略对于癌症转移的预防至关重要。
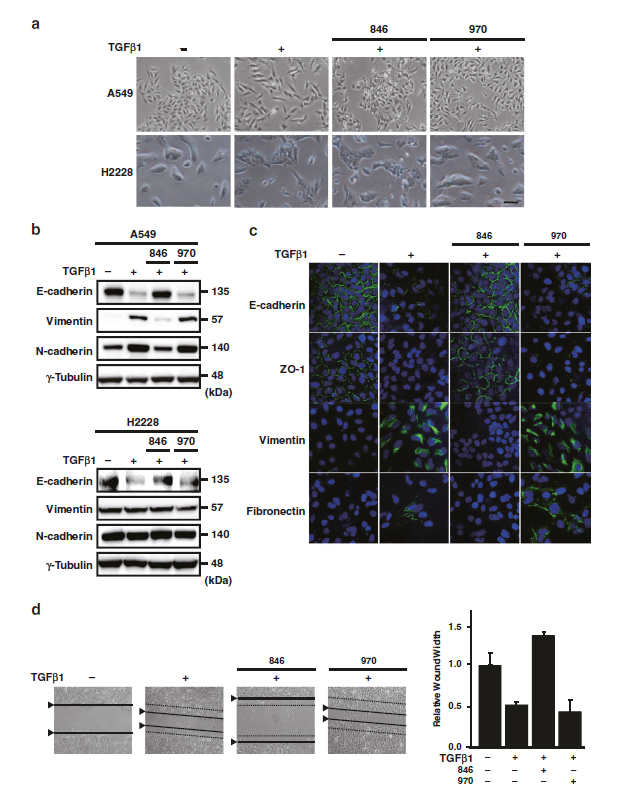
NCB-0846抑制TGFβ1诱导的EMT进程
TNIK是β-catenin/TCF4转录复合物的组成成分,对于Wnt靶基因的转录至关重要。研究人员前期开发了能够抑制TNIK的小分子化合物NCB-0005。该研究旨探究NCB-0846对TGFβ1诱导的肺癌EMT进程的影响。
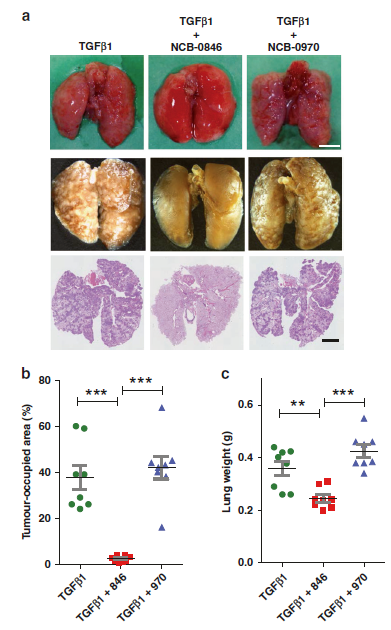
NCB-0846抑制肺癌细胞的转移
研究人员发现,NCB-0846能够抑制TGFβ1诱导的A549细胞的EMT进程。该抑制作用与SMAD2/3蛋白的磷酸化和核转运相关。 通过尾静脉注射免疫缺陷型小鼠发现,NCB-0846能够抑制TGFβ1诱导的A549细胞的肺转移。进一步的研究显示,EMT的抑制作用是通过抑制TGFBR1(I型TGFβ受体)基因所介导的,而该作用有一部分是通过诱导靶向TGFBR1转录的的microRNA(miR-320和miR-186)实现的。
总而言之,该研究结果显示,NCB-0846能够通过在转录水平上下调TGFBRI的表达,从而阻断TGFβ/SMAD信号转导通路和抑制肺癌细胞的EMT进程,该研究也提供了一种潜在的有希望的预防肺癌患者转移的方法。
原始出处:
Sugano, T., Masuda, M., Takeshita, F. et al. Pharmacological blockage of transforming growth factor-β signalling by a Traf2- and Nck-interacting kinase inhibitor, NCB-0846. Br J Cancer (27 November 2020).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#阻断#
26
#抑制剂#
37
#TGF#
32
#Smad#
37
#TGFβ#
32
#SMA#
29
#信号通路#
34
在EMT进程中,癌细胞失去上皮细胞的粘附/极性并获得间充质特性。EMT增加了细胞的可塑性和运动性,从而促进肿瘤细胞离开其原生部位,通过全身循环,并在远端重建肿瘤
79
赞
78
EMT的作用
73