Hypertension:较高的血浆醛固酮浓度与主动脉夹层和动脉瘤风险升高有关
2022-02-01 MedSci原创 MedSci原创
较高的PAC与高血压患者主动脉夹层和动脉瘤几率增加相关,即使在没有原发性醛固酮增多症的情况下,这意味着PAC可能是高血压患者主动脉夹层和动脉瘤预防的目标。
动物模型表明循环醛固酮水平会导致主动脉夹层和动脉瘤,然而缺乏来自人群的数据。

近日,心血管权威杂志Hypertension上发表了一篇研究文章,研究人员旨在评估血浆醛固酮浓度(PAC)与主动脉夹层和动脉瘤之间的关系。
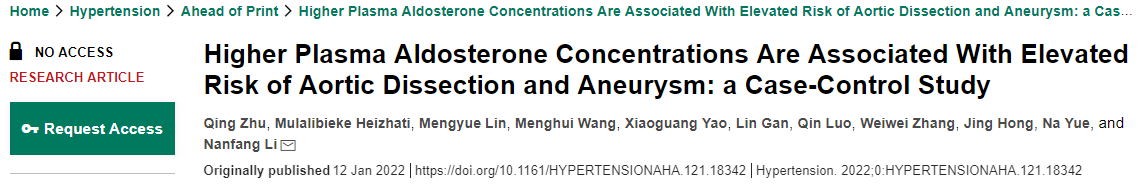
研究人员从基于医院的电子数据库中识别出患有主动脉夹层和动脉瘤且在疾病发作前评估PAC的患者,并将其设置为病例组。同时,研究人员根据病例组的年龄和性别匹配了进行PAC测量但没有主动脉夹层和动脉瘤的对照组,匹配比例为1:4。多变量logistic回归分析用于评估PAC与主动脉夹层和动脉瘤之间的关系。
在2004年至2021年期间,共有133例病例和531名对照者(均为高血压)入组,其中男性占77.9%,平均年龄为55.5岁,PAC为13.9ng/dL。病例组的PAC(14.51 vs. 13.65ng/dL,P=0.012)显著高于对照组。在Logstic回归分析中,较高的PAC使主动脉夹层和动脉瘤的几率增加1.68倍(95%CI为1.14-2.48,P=0.008),在调整模型中显著(比值比为1.69[95%CI为1.11-2.57],P=0.015)。在分层分析中,所有年龄的女性和患有冠状动脉疾病的男性中都观察到了两者之间的关联。通过排除PAC测量中干扰剂和原发性醛固酮增多症患者的敏感性分析并没有改变两者之间的关系。
由此可见,较高的PAC与高血压患者主动脉夹层和动脉瘤几率增加相关,即使在没有原发性醛固酮增多症的情况下,这意味着PAC可能是高血压患者主动脉夹层和动脉瘤预防的目标。
原始出处:
Qing Zhu.et al.Higher Plasma Aldosterone Concentrations Are Associated With Elevated Risk of Aortic Dissection and Aneurysm: a Case-Control Study.Hypertension.2022.https://www.ahajournals.org/doi/10.1161/HYPERTENSIONAHA.121.18342
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#PE#
40
#TENS#
44
#醛固酮#
35
#主动脉#
31
#Hypertension#
30
#动脉夹层#
35
#浓度#
38
好文章,值得一读。
52
认真学习了
61