Clin Cancer Res:早早使用大剂量激素管理irAE与抗PD-1单药治疗晚期黑色素瘤的预后不良相关
2021-08-12 Nebula MedSci原创
早早使用大剂量激素管理irAE与抗PD-1单药治疗晚期黑色素瘤的预后不良相关
程序性细胞死亡受体-1 (PD-1)抑制剂是晚期黑色素瘤的一线治疗方法。严重的免疫相关不良反应(ieAE)通常需要糖皮质激素(GCC)免疫抑制治疗。但是,在抗PD-1单药治疗过程中,GCC的使用及其与患者生存预后的相关性尚未明确。
这是一项多中心的回顾性分析,纳入了2009年至2019年期间采用抗PD-1单克隆疗法治疗的患者,从5个独立的队列中采集详细的GCC使用数据。中位随访时间为206周。从抗PD-1治疗开始跟踪irAE,直到病情进展、开始新的治疗或随后一次随访。最后还分析了irAE、GCC使用和存活预后的相关性。
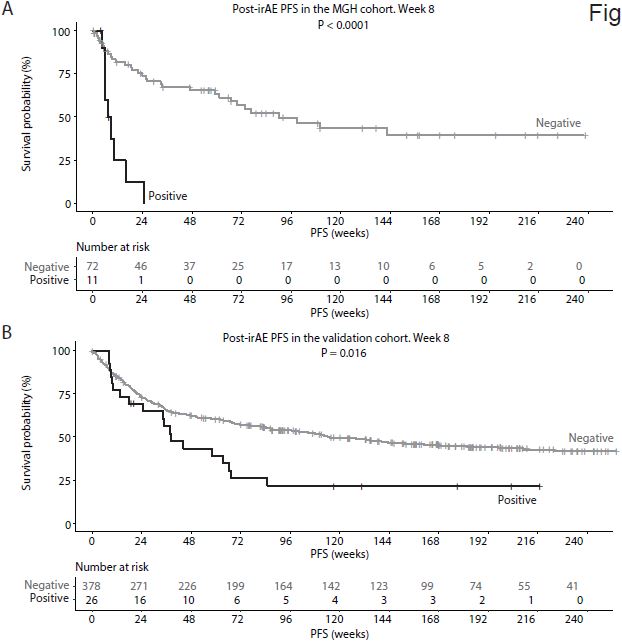
MGH队列和验证队列两组患者的PFS
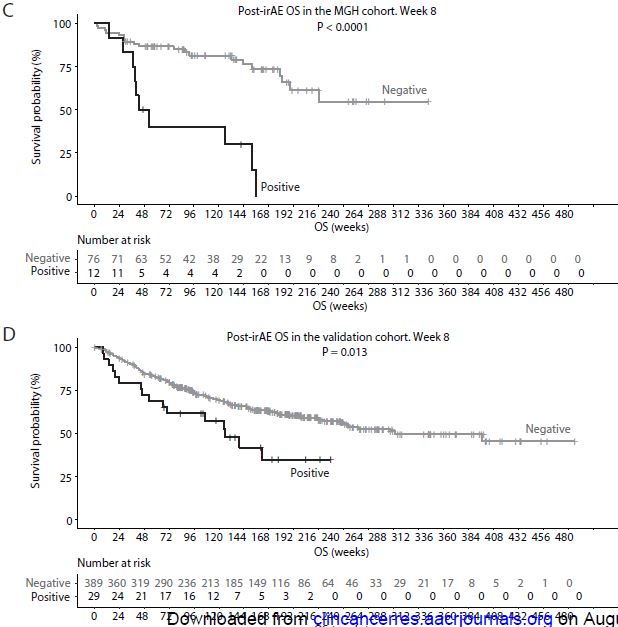
在总队列947位患者中,509位(54%)患者发生了irAE。在MGH队列(irAE[+]n=90)中,与未早期使用大剂量GCC的irAE相比,使用了大剂量GCC(≥60 mg,强的松)的早发型irAE(抗PD-1治疗后的前8周内)与irAE后的PFS和OS较差独立相关 (irAE后 PFS: HR 5.37, 95%CI 2.10-13.70, p<0.001; OS: HR 5.95, 95%CI 2.20-16.09, p<0.001)。
MGH队列和验证队列两组患者的OS
上述研究结果在联合验证队列中得到了证实(irAE[+]n=419, irAE后 PFS: HR1.69, 95%CI 1.04-2.76, p=0.04; OS: HR 1.97, 95%CI 1.15-3.39, p=0.01)。此外,在irAE后PFS的26周重要分析中,观察到了相似的结果,但在irAE后OS的26周分析中未观察到相似的结果。采用累积GCC暴露量为测量的敏感性分析也获得了相似的结果。
综上,irAE发生后,早早使用大剂量GCC与不良PFS和OS预后相关。在抗PD-1单药治疗过程中,应更理智的应用GCC。需要开展前瞻性的随机对照临床试验进一步验证该研究结果。
原始出处:
Xue Bai, Jiani Hu, Allison Betof Warner, et al. Early use of high-dose-glucocorticoid for the management of irAE is associated with poorer survival in patients with advanced melanoma treated with anti-PD-1 monotherapy. Clin Cancer Res August 10 2021 DOI:10.1158/1078-0432.CCR-21-1283
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#单药治疗#
43
#色素#
26
#预后不良#
37
#黑色素#
40
#黑色素#
36
#大剂量#
42
每日一看~
49