Br J Cancer:10种实体瘤患者诊断时肿瘤分期的社会人口统计学差异及其对人群的影响
2021-02-16 xiaozeng MedSci原创
诊断疾病处于非晚期阶段的患者已成为目前癌症预防和控制策略的主要手段,是对癌症的预防和筛查的一个补充。
诊断疾病处于非晚期阶段的患者已成为目前癌症预防和控制策略的主要手段,是对癌症的预防和筛查的一个补充。然而,大多数的癌症患者是在症状发作后才被诊断出来的,其原因归结于只有少数癌症可以进行有效的筛查。
因此,除了优化筛查工作外,许多国家的公共卫生政策还注重于缩短从症状发作到诊断的间隔时间,以实现降低晚期癌症人群。
既往研究显示,癌症患者确诊时疾病的阶段预示着患者的存活情况,且了解相关的统计学差异现象可以较好的指导疾病的干预措施。
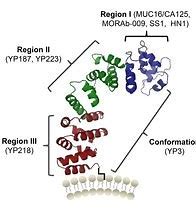
肿瘤部位分层模型中按年龄(30-99岁)分布的诊断晚期的调整优势比
英国政府在2018年制定了一个目标,即在2028年前实现75%的普通实体瘤患者的TNM分期为I/II期。然而,该目标如何实现,如何更好的改善患者的TNM分期仍具挑战,而有助于改善患者肿瘤诊断分期分布的策略是减少社会人口统计时差异性现象的发生。
该研究通过分析10种实体瘤(乳腺癌、膀胱癌、结肠癌、子宫内膜癌、肺癌、黑素瘤、前列腺癌、直肠癌、肾癌和卵巢癌)患者的诊断情况,分析III/IV与I/II期的社会人口统计学差异。旨在研究英国近期常见癌症的诊断分期以及相关社会人口统计学变异,并提供有关患者诊断分期的高度完整的信息。
消除年龄、性别和收入不平衡的影响
结果显示,在202,001例病例中,有57%诊断时为I/II期(相比于75%的目标仍有18%的“差距”)。尽管癌症部位是以上结果的一大主因,但研究人员发现,诊断为III/IV期的可能性随年龄增加而升高,其中前列腺癌和子宫内膜癌最显著。
在除肺癌和肾癌以外的所有部位,患者的经济收入状况与诊断时的阶段相关。而其中的四种癌症表现出性别的不平衡。通过消除社会人口统计学的不平等现象,研究人员最终分析得到,在患有10种实体瘤的患者中有61%的患者诊断时为I/II期,从而将目标差距缩小到14%。
总而言之,该研究结果显示,通过潜在的消除社会人口统计学上的不平等现象,能为实现阶段性目标做出一定的贡献。此外,研究人员建议早期的诊断策略应关注整个人群,而不只是高风险的社会人口统计学人群。
原始出处:
Barclay, M.E., Abel, G.A., Greenberg, D.C. et al. Socio-demographic variation in stage at diagnosis of breast, bladder, colon, endometrial, lung, melanoma, prostate, rectal, renal and ovarian cancer in England and its population impact. Br J Cancer (09 February 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#肿瘤分期#
37
#统计学#
29
#社会#
41
😀😀
0