葛兰素史克(GSK)和Medicago推出植物来源的COVID-19疫苗
2021-03-18 Allan MedSci原创
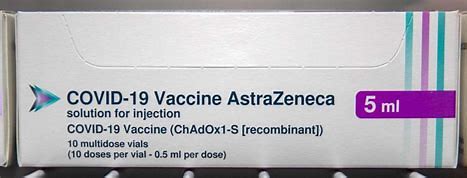
葛兰素史克(GSK)和加拿大生物制药公司Medicago已针对其佐剂植物来源的COVID-19候选疫苗启动了III期试验。
葛兰素史克(GSK)和加拿大生物制药公司Medicago已针对其佐剂植物来源的COVID-19候选疫苗启动了III期试验。候选疫苗使用冠状病毒样颗粒(CoVLP)技术,该技术由重组刺突(S)糖蛋白组成,表达为病毒样颗粒(VLP),与GSK的植物来源佐剂一起给药。

Medicago表示已获得加拿大和美国监管机构的批准,根据“ II期中期阳性结果”开始将健康成年人纳入III期试验。
2021年2月,佐剂植物源疫苗候选者获得了美国食品药品监督管理局(FDA)的快速通关称号。
研究的第三阶段部分将评估佐剂型CoVLP制剂的功效和安全性,并将招募多达30,000名参与者。最初,该试验将招募18至65岁的健康成年人,然后招募65岁以上的老年人和具有合并症的成年人。
两家公司补充说,该疫苗的II期试验已接近尾声,预计结果将于2021年4月公布。
Medicago首席执行官兼总裁Takashi Nagao表示:“我们很高兴迈出重要一步,在全球各地启动了III期临床试验。这使我们离提供重要的新COVID-19疫苗更近了一步”。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#DIC#
26
#植物#
35
#葛兰素史克#
34
#Med#
18
优势在哪里?
75
看临床用了以后的
68