RET抑制剂TPX-0046治疗肿瘤,I/II期SWORD-1期研究已取得初步临床数据
2021-04-06 Allan MedSci原创
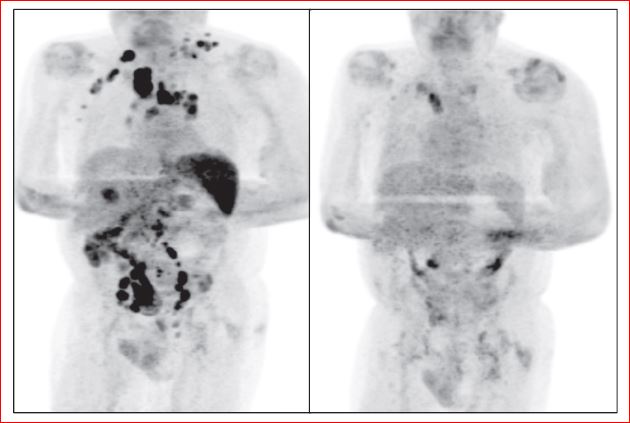
在5例未行RET TKI的患者中,有4例显示肿瘤消退率为-42%、-37%、-23%和-3%。在9例接受TKI治疗的患者中,有3例患者的肿瘤消退率为-44%、-27%和-17%。
Turning Point Therapeutics是一家精密肿瘤学公司,致力于开发针对癌症遗传驱动力的下一代疗法,Turning Point Therapeutics今天报告了正在进行的RET抑制剂TPX-0046的I/II期SWORD-1期研究的初步临床数据。
该研究的I期剂量寻找部分的初步数据显示出初步的临床活性,包括客观反应和普遍耐受良好的安全性。Turning Point Therapeutics继续评估剂量和时间表,以确定II期剂量,并计划修订研究方案。
纪念斯隆·凯特琳医院癌症中心早期药物开发服务部总经理Alexander Drilon说:“在美国和欧盟,每年由RET驱动的癌症会影响到近10,000名患者,而使用选择性RET抑制剂治疗后进展的患者仍然得不到足够的治疗。TPX-0046的初步数据令人鼓舞,其总体安全性和有效性良好”。
纳入研究的21位患者包括10例非小细胞肺癌(NSCLC)和11例甲状腺髓样癌(MTC)。所有16名接受TKI(酪氨酸激酶抑制剂)治疗的患者先前均接受了选择性RET TKI治疗,而9名患者(56%)接受了1种以上的TKI治疗。91%(19/21)的患者的ECOG基线表现评分为1,近一半(10/21)的患者接受了3种或更多的先前疗法。
在5例未行RET TKI的患者中,有4例显示肿瘤消退率为-42%、-37%、-23%和-3%。在9例接受TKI治疗的患者中,有3例患者的肿瘤消退率为-44%、-27%和-17%。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#临床数据#
46
#Word#
41
#抑制剂#
40
#RET#
56
#RET抑制剂#
47
已看,还可以。
89