J Clin Oncol:以达雷木单抗联合疗法治疗多发性骨髓瘤的持续性MRD阴性情况(POLLUX和CASTOR)
2021-02-01 MedSci原创 MedSci原创
与标准疗法相比,以达雷木单抗为基础的联合方案可诱导更高的持续性MRD阴性率。
在POLLUX(达雷木单抗/来那度胺/地塞米松[D-Rd])和CASTOR(达雷木单抗/硼替佐米/地塞米松[D-Vd])试验中,达雷木单抗将复发性/难治性多发性骨髓瘤患者进展或死亡的风险均降低了60%以上。最小残留病灶(MRD)是疾病控制的一种敏感性检测方法。本研究旨在评估持续性MRD阴性与多发性骨髓瘤患者预后的相关性。
在这两项研究中,在疑似完全缓解(CR)、确诊CR(POLLUX)后3个月和6个月、第一剂药后6个月和12个月以及CR后每12个月时,采用二代测序(10-5)评估患者的MRD情况。在意向治疗人群(ITT)和≥CR人群中评估持续性MRD阴性(≥6个月或≥12个月)。
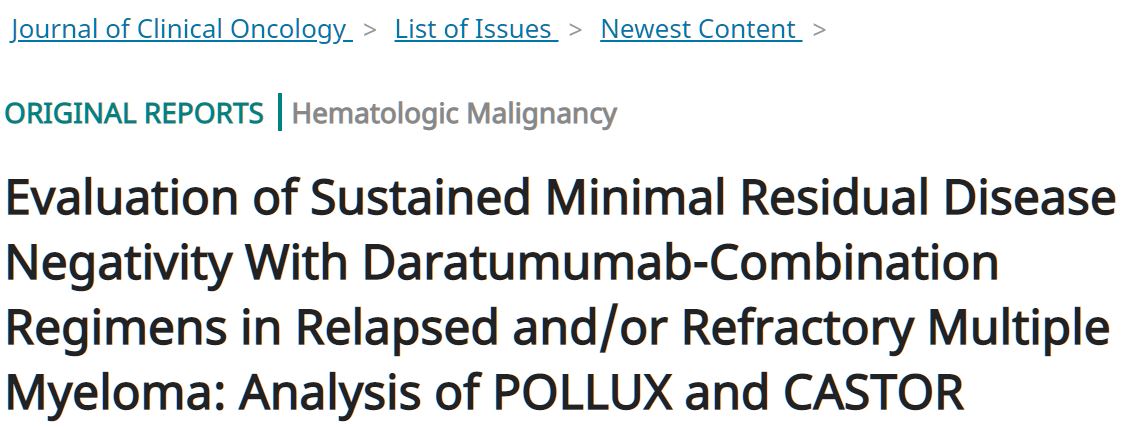
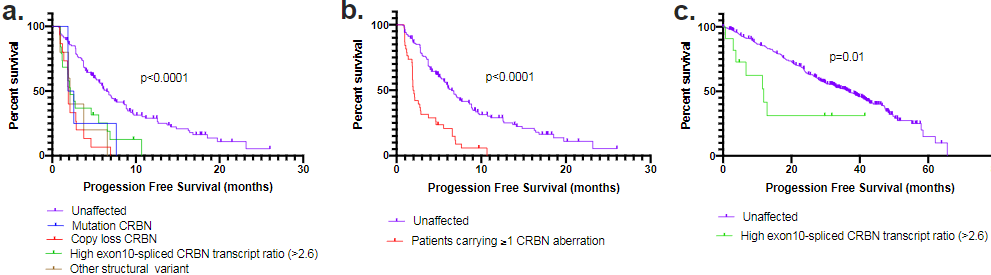
不同MRD状态的患者PFS
POLLUX试验中位随访了54.8个月,CASTOR试验中位随访了50.2个月。在ITT人群中,采用D-Rd vs 来那度胺和地塞米松(Rd)治疗的患者的MRD阴性率为32.5% vs 6.7%;采用D-Vd vs 硼替佐米和地塞米松(Vd)治疗的患者的MRD阴性率为15.1% vs 1.6%(两组p<0.0001)。获得≥CR患者的MRD阴性率更高:D-Vd vs Rd=57.4% vs 29.2(p=0.0001),D-Vd vs Vd=52.8% vs 17.4%(p=0.0035)。
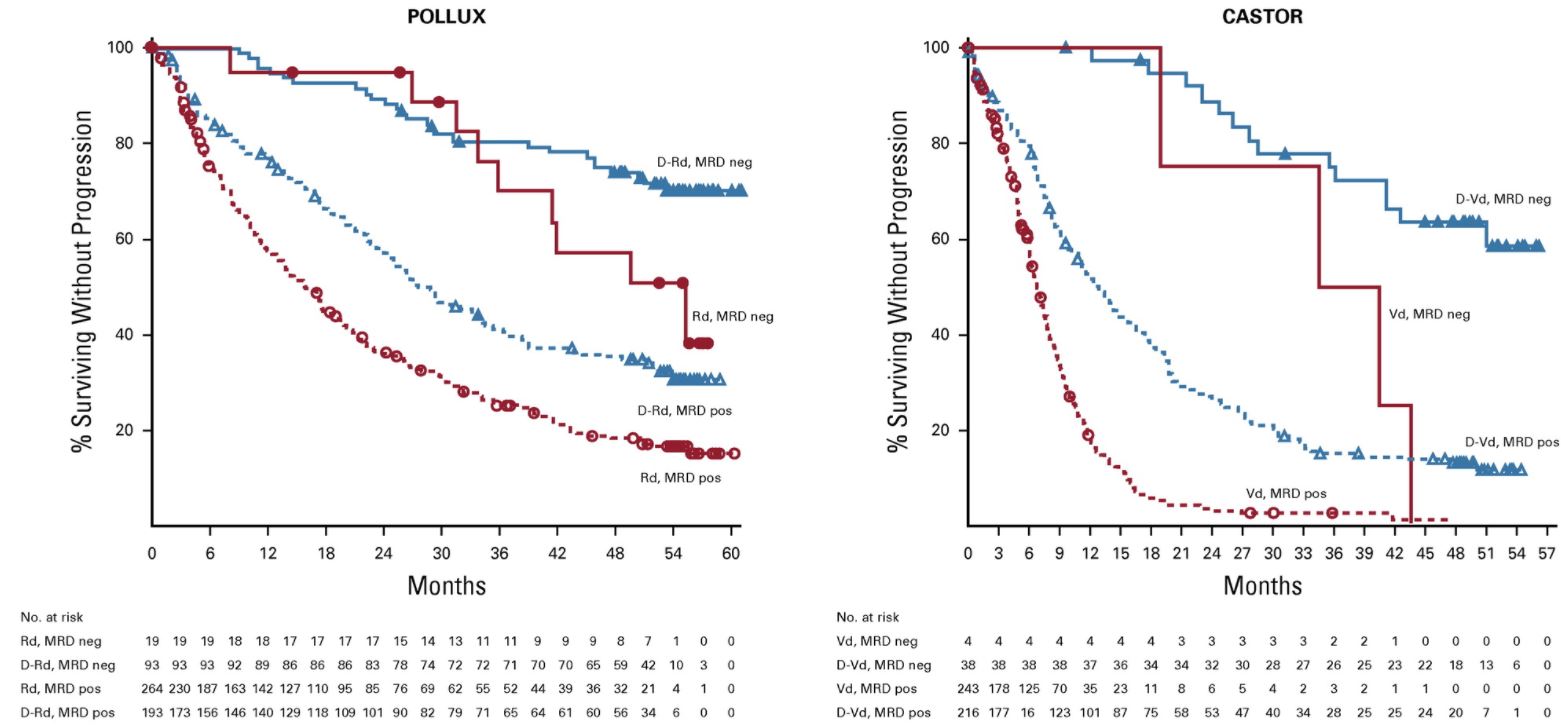
持续MRD阴性(>6个月)患者的PFS
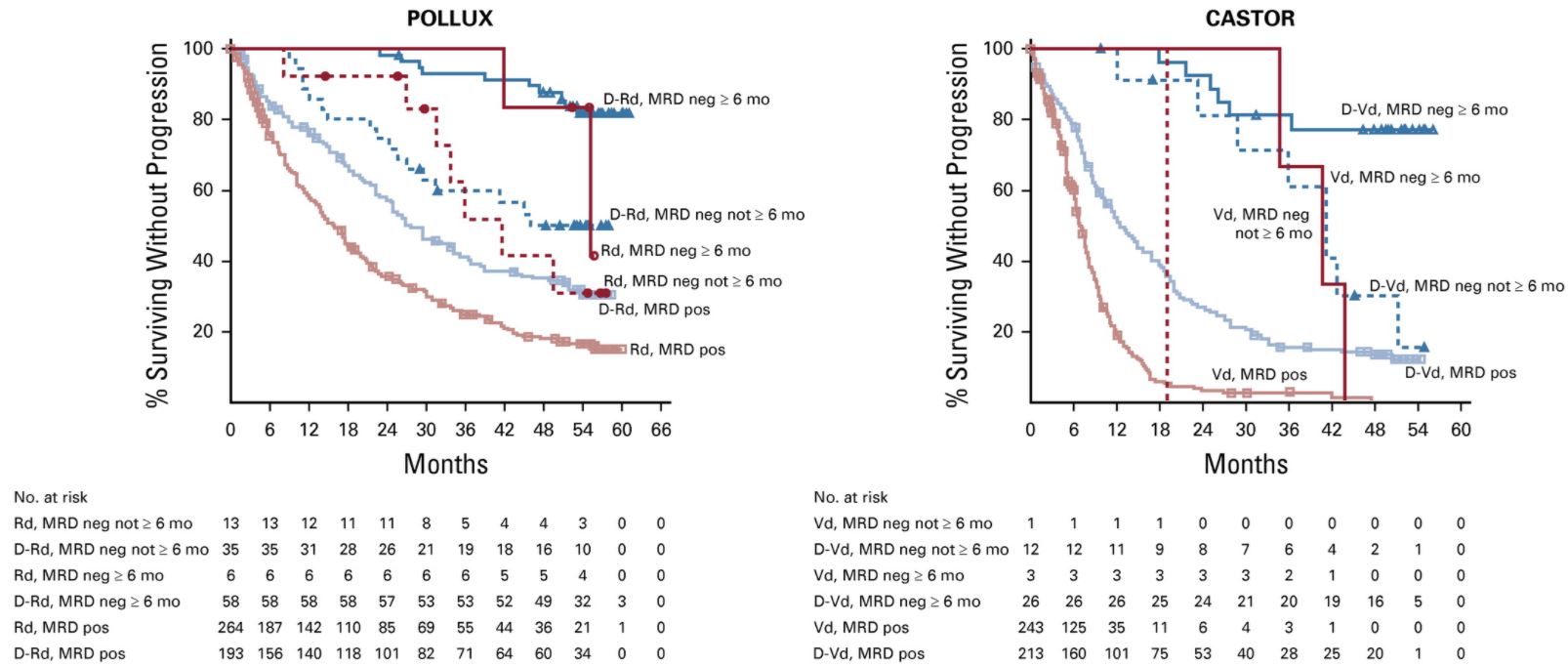
持续MRD阴性(>12个月)患者的PFS
在ITT人群中,D-Rd组获得持续MRD阴性超过6个月和12个月的患者比例均明显高于Rd组(20.3% vs 2.1%和16.1% vs 1.4%);D-Vd组获得持续MRD阴性超过6个月和12个月的患者比例也均明显高于Vd组(10.4% vs 1.2%和6.8% vs 0%)。在≥CR患者中也观察到了类似的持续性MRD阴性结果。在包含达雷木单抗的治疗组中,更多的患者获得MRD阴性和持续的MRD阴性,这与患者的无进展存活期延长相关。
总之,与标准疗法相比,以达雷木单抗为基础的联合方案可诱导更高的持续性MRD阴性率,而持续性MRD阴性与持久的缓解和临床存活期延长相关。
原始出处:
Herve Avet-Loiseau, et al. Evaluation of Sustained Minimal Residual Disease Negativity With Daratumumab-Combination Regimens in Relapsed and/or Refractory Multiple Myeloma: Analysis of POLLUX and CASTOR. Journal of Clinical Oncology. January 29, 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Oncol#
33
#AST#
35
#持续性#
67
#多发性#
41
#联合疗法#
26
#MRD#
33
#达雷木单抗#
30
#Cas#
0
谢谢梅斯分享这么多精彩信息
46