NEJM:心源性休克患者治疗优先选择米力农还是多巴酚丁胺?
2021-08-05 MedSci原创 MedSci原创
在心源性休克患者中,米力农和多巴酚丁胺治疗在主要复合结局或重要次要结局方面没有显著差异。
心源性休克与发病率和死亡率相关。尽管正性肌力支持是心源性休克药物治疗的主要支柱,但几乎没有证据可以指导临床实践中正性肌力药物的选择。
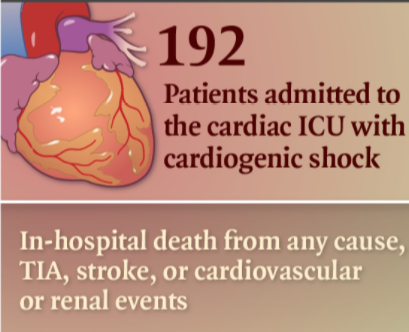
近日,顶级医学期刊NEJM上发表了一篇研究文章,研究人员以双盲方式随机分配心源性休克患者接受米力农或多巴酚丁胺治疗。该研究的主要结局是院内任何原因死亡、心脏骤停复苏、接受心脏移植或机械循环支持、非致死性心肌梗死、短暂性脑缺血发作或神经科医生诊断的卒中,或开始肾脏替代治疗的复合结局。该研究的次要结局包括主要复合结局的各个组成部分。
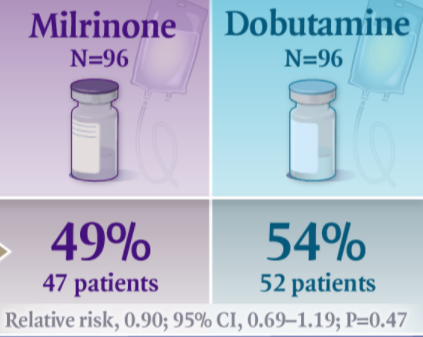
该研究共招募了192名参与者(每组96名)。治疗组在主要结局方面没有显著差异;米力农组47名参与者(49%)和多巴酚丁胺组52名参与者(54%)发生主要结局事件(相对风险为0.90;95%置信区间[CI]为0.69至1.19;P=0.47)。
两组间在次要结局方面也没有显著差异,包括院内死亡(分别为37%和43%的参与者;相对风险为0.85;95%CI为0.60至1.21)、复苏的心脏骤停(7%和9%;风险比为0.78;95%CI为0.29至2.07),接受机械循环支持(12%和15%;风险比为0.78;95%CI为0.36至1.71),或开始肾脏治疗替代疗法(22%和17%;风险比为1.39;95%CI为0.73至2.67)。
由此可见,在心源性休克患者中,米力农和多巴酚丁胺治疗在主要复合结局或重要次要结局方面没有显著差异。
原始出处:
Rebecca Mathew,et al.Milrinone as Compared with Dobutamine in the Treatment of Cardiogenic Shock.NEJM.2021.https://www.nejm.org/doi/full/10.1056/NEJMoa2026845
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#米力农#
35
#心源性休克#
54
#心源性#
31
领先世界,为临床工作者提供学习的平台
59
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
65
学习了
55
学习
60
学习了
54