Hypertension:颈动脉血压波形的固有频率可预测心力衰竭
2021-01-06 MedSci原创 MedSci原创
新的IF可能是社区人群心力衰竭风险的重要标志。
来自于动脉波形的固有频率(IF)与心血管功能、衰老和心血管疾病(CVD)相关。然而,这些新指标的预后价值尚未明确。近日,心血管权威杂志Hypertension上发表了一篇研究文章,研究人员旨在评估IF与CVD风险之间的关系。
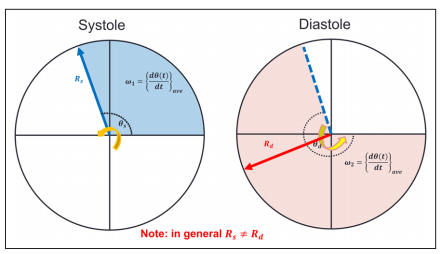
该研究的样本来自弗莱明翰心脏研究的原始样本、子代样本和第三代样本,并纳入了基线时无CVD的参与者(N=4700;平均年龄为52岁,女性占55%)。研究人员直接从一系列颈动脉压力波中提取了2个主要频率:收缩期心血管系统耦合的IF(ω1)和舒张期心血管系统解耦合的IF(ω2)。总频率差异(Δω)定义为ω1和ω2之差。研究人员使用Cox比例风险回归模型将IF与平均随访10.6年的CVD事件相关联。
在针对CVD危险因素进行调整的多变量模型中,较高的ω1(风险比[HR]为1.14 [95%CI为1.03–1.26];P=0.01)和Δω(HR为1.16 [95%CI为1.03-1.30];P=0.02),但较低的ω2(HR为0.87 [95%CI为0.77-0.99];P=0.03)与较高复合CVD事件发生风险相关。
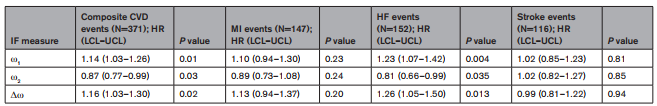
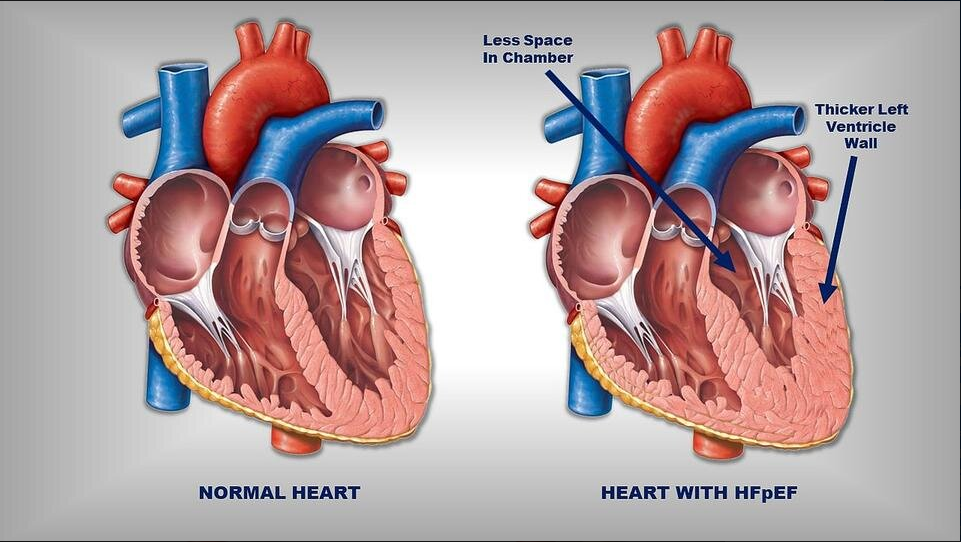
在经过类似调整的模型中,较高的ω1(HR为1.23 [95%CI为1.07–1.42];P=0.004)和Δω(HR为1.26 [95%CI为1.05-1.50];P=0.01),但较低的ω2(HR为0.81 [95%CI为0.66-0.99]; P=0.04)与较高的心力衰竭风险相关。IF与心肌梗塞或卒中发生无明显相关性。
由此可见,新的IF可能是社区人群心力衰竭风险的重要标志。
原始出处:
Leroy L. Cooper.et al.Intrinsic Frequencies of Carotid Pressure Waveforms Predict Heart Failure Events The Framingham Heart Study.Hypertension.2021.https://www.ahajournals.org/doi/10.1161/HYPERTENSIONAHA.120.15632
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#PE#
40
有意思的研究
52
#动脉血#
45
#颈动脉#
33
#TENS#
37
#学习#
72
#Hypertension#
21
学习了#心血管#
120