JAHA:重症监护患者右心室肺动脉耦联与死亡率的关系
2021-03-29 MedSci原创 MedSci原创
较低的TASV/RVSP比值与心脏重症监护病房患者的短期和长期死亡率增加相关,这些结果提示了RV肺动脉耦连受损作为不良预后的决定因素的重要性。
右心室(RV)肺动脉耦联受损与慢性心脏病患者较高的死亡率相关,但很少有研究对重症患者进行评估。

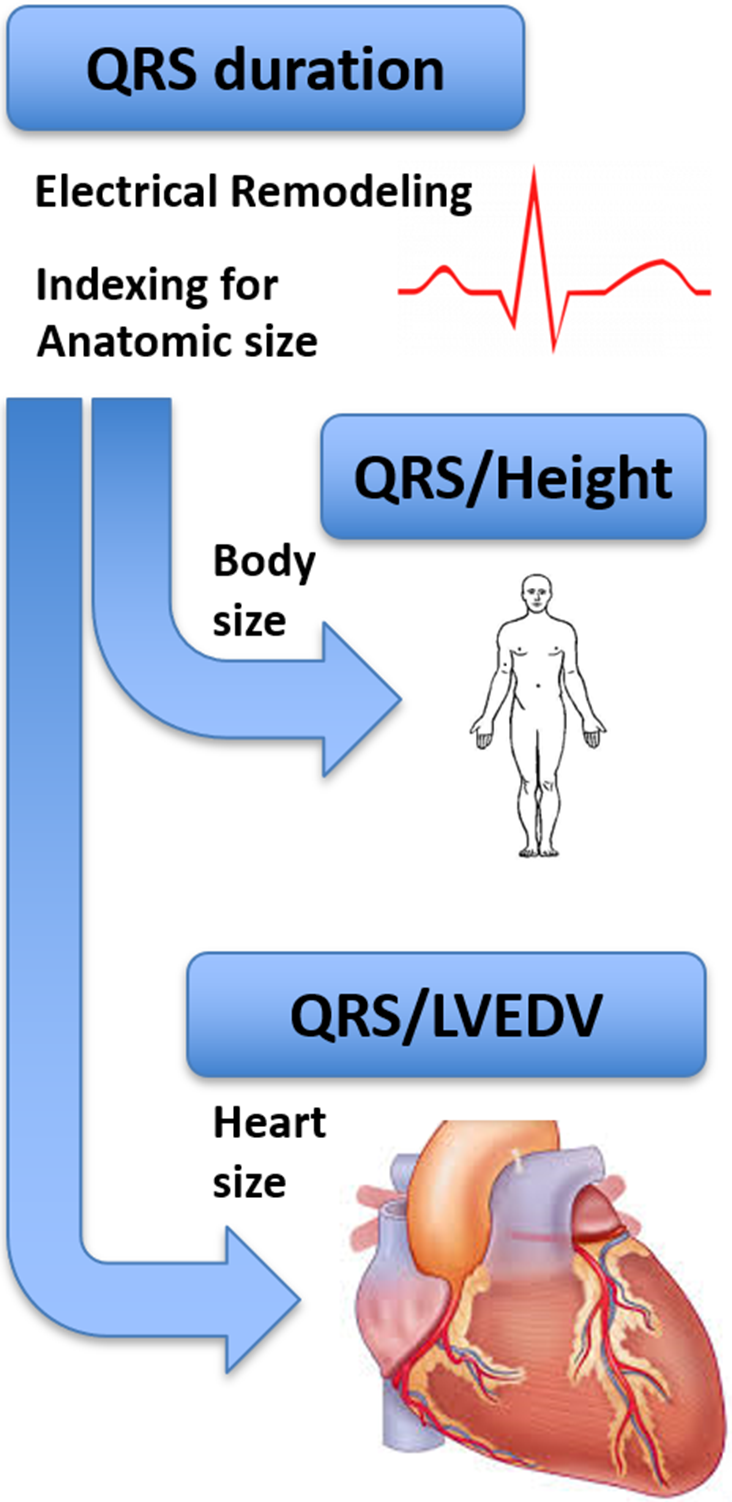
近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,在这项研究中,研究人员试图评估心脏重症监护病房患者RV肺动脉耦联(由三尖瓣环形收缩峰值组织多普勒速度(TASV)/估算的RV收缩压(RVSP)之比来定义)与死亡率之间的相关性。
研究人员使用2007年至2018年期间心脏重症监护病房住院数据库,纳入了在住院1天内测得的TASV/RVSP比值的患者。研究人员使用多因素logistic回归分析住院死亡率,并使用多变量Cox比例风险分析法分析了患者1年死亡率。

研究人员纳入了4259名平均年龄为69±15岁的患者(女性占40.1%)。56%参与者入院诊断为急性冠状动脉综合征,52%为心力衰竭,24%为呼吸衰竭和12%为心源性休克。平均TASV/RVSP比值为0.31±0.14,7%的患者住院死亡。较高的TASV/RVSP比值与较低的住院死亡率(校正后的单位比值比为0.68;95%CI为0.58-0.79;P<0.001)和住院幸存者的1年死亡率降低(调整后的风险比为0.83;95%CI为0.77-0.90;P<0.001)相关。在TASV/RVSP比值五分位数每增加一个分位数,研究人员观察到受试者住院率和1年死亡率逐步降低。调整左心室收缩和舒张功能后,TASV/RVSP比值与死亡率之间的相关性仍然显著。
由此可见,较低的TASV/RVSP比值与心脏重症监护病房患者的短期和长期死亡率增加相关,这些结果提示了RV肺动脉耦连受损作为不良预后的决定因素的重要性。需要进一步的研究以明确优化RV肺动脉耦联的干预措施是否可以改善患者结局。
原始出处:
Jacob C. Jentzer.et al.Right Ventricular Pulmonary Artery Coupling and Mortality in Cardiac Intensive Care Unit Patients.J AM HEART ASSOC.2021.https://www.ahajournals.org/doi/full/10.1161/JAHA.120.019015
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#重症监护患者#
33
不错
55
#AHA#
29
#右心室#
33
#监护#
37
有意义
71
123
67