2021 ACR:膝关节骨关节炎的超声评估及其与X射线的一致性
2021-11-27 MedSci原创 MedSci原创
本研究旨在1) 表征膝关节OA的超声特征及其与疼痛和功能水平的关系,以及2)确定超声与常规X射线在膝关节OA评估中的相关性和一致性。
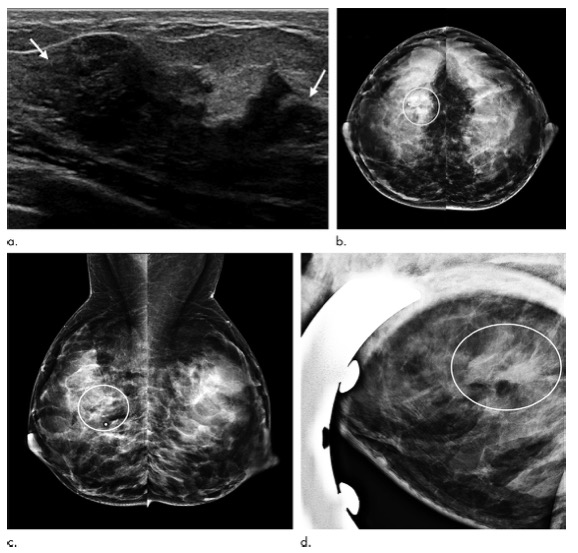
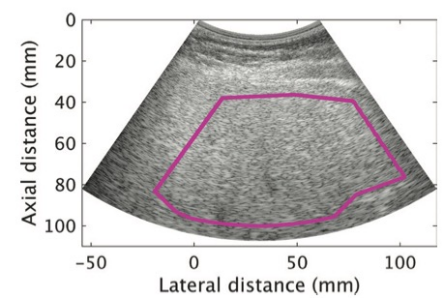
超声检查(US)已越来越多地用于评估各种肌肉骨骼状况。然而,US在临床实践中诊断骨关节炎(OA)的价值仍不清楚。本研究旨在1) 表征膝关节OA的超声特征及其与疼痛和功能水平的关系,以及2)确定超声与常规X射线在膝关节OA评估中的相关性和一致性。

方法:2018年8月至2019年8月期间,在Cho Ray医院风湿科门诊对145名40岁及以上(83.4%女性)、平均年龄为61.7岁、临床诊断为原发性膝关节OA的患者进行横断面研究。排除伴有炎症性关节病的患者。使用视觉模拟量表(VAS) 进行临床疼痛评估,使用西安大略和麦克马斯特大学关节炎指数 (WOMAC)对所有受试者的功能状态进行评估,接受膝关节X光和US检查。研究了超声检查结果与临床和放射学特征之间的相关性。
共评估了290个膝关节。US最常见的特征是软骨厚度降低(74.5%)、骨赘 (66.9%)、积液(55.9%)、内侧半月板挤压(78.6%)、外侧半月板挤压(39.3%)、滑膜增厚 (17.2%) )和贝克囊肿(15.2%)。VAS和WOMAC疼痛评分与US测量的积液水平和骨赘大小呈正相关,与股骨内侧软骨厚度呈负相关。超声内侧软骨厚度与X线内侧关节间隙宽度(rs = 0.3,p < 0.01)以及超声和X线骨赘分级之间呈正相关(内侧和外侧关节间隙分别为rs = 0.69,p < 0.01和rs = 0.47,p < 0.01)。129个 (44.5%)膝盖在超声和X光片上均发现骨赘,44个(34.1%)膝盖只在US检查中发现骨赘,17个(13.2%) 膝仅在X光检查中发现骨赘 (Kappa = 0.58;p < 0.01)。
这些结果支持超声检查与传统X线相比在评估膝关节OA病变方面的有效性。此外,在检测膝关节OA的早期变化(如软骨损伤和轻度骨赘)方面,超声似乎比X射线更敏感。
原始出处:
Nguyen K, Tran D. Ultrasonographic Assessment of Knee Osteoarthritis and Its Agreement with Radiography [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 10).

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#超声评估#
38
#骨关节#
56
#一致性#
38
#X射线#
37
#学习#
60
#关节炎#
30
#ACR#
33
#膝关节骨关节炎#
48