Journal for immunotherapy of cancer:肝脏如何通过大脑调控饮食?脂质信号或通过下丘脑实现的
2022-06-30 周科 神经周K
Autotaxin (ATX) 是一种分泌型糖蛋白,主要生理功能是以溶血磷脂酰胆碱(LPC)为底物催化生成溶血磷脂酸(LPA)。外周能量代谢可影响大脑神经元活性。
溶血磷脂酸(LPA)在突触神经传递和可塑性中起着重要的调节作用。大脑LPA的合成取决于其前体溶血磷脂酰胆碱(LPC),LPC主要由肝脏分泌,在激活后通过血脑屏障进入大脑中。LPA通过激活突触前LPA2受体,调节谷氨酸释放,最终可调控神经元兴奋性。
Autotaxin (ATX) 是一种分泌型糖蛋白,主要生理功能是以溶血磷脂酰胆碱(LPC)为底物催化生成溶血磷脂酸(LPA)。外周能量代谢可影响大脑神经元活性。

2022年6月27日德国科隆大学Johannes Vogt?研究团队揭示了外周肝脏来源的LPA通过下丘脑促进食欲的神经元调控摄食行为。
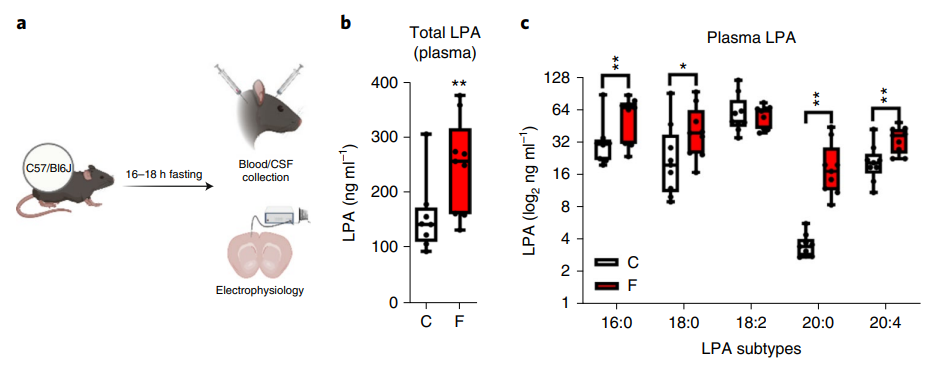
图1:禁食后血清LPA水平增加
研究人员发现禁食16小时到18小时的小鼠血清和脑脊液中LPA水平增加,皮层微小兴奋性突触后电流增强。抑制ATX活性阻断 LPA合成后,这种增强谷氨酸能突触传递作用完全消失。原位杂交实验发现ATX主要表达在皮层和海马区域。
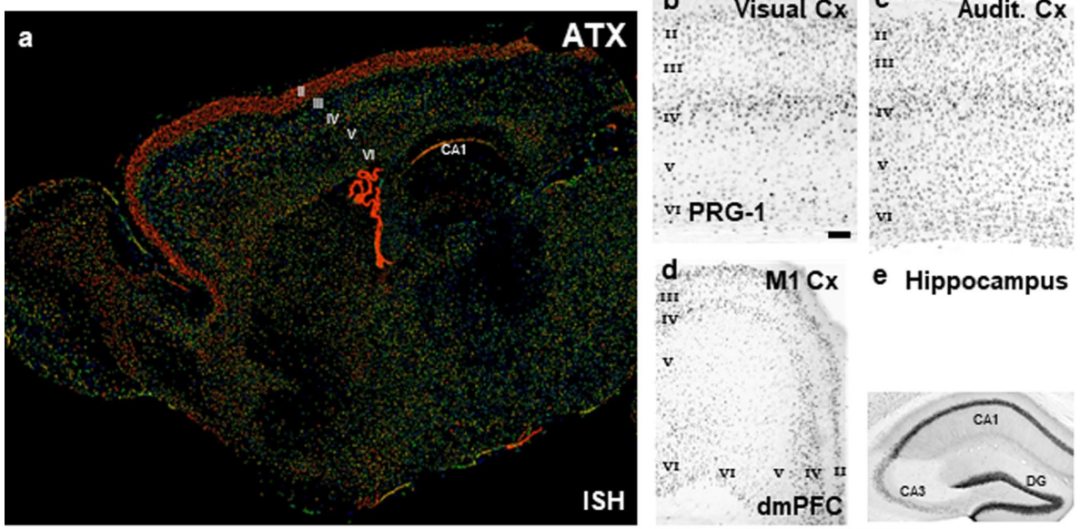
图2:原位杂交发现ATX在大脑中的表达
在新物体探索实验中,(与正常饮食小鼠相比)禁食小鼠对新物体探索行为增加,在抑制LPA合成或敲除突触前LPA2受体后可减弱对新物体的探索行为。
可塑性相关基因蛋白PRG-1在突触间隙摄取LPA,实现对LPA的再回收。PRG-1主要表达在皮层神经元上。通过基因工程技术突变PRG-1后减少LPA的突触间隙再摄取,引起LPA水平的增加,这可进一步增强禁食引起的新物体探索行为。
禁食后小鼠再次进食普通饲料或高脂饲料后饮食增多,表现贪食行为,体重增加。PRG-1突变后可进一步强化禁食后引起的贪食行为,也就是小鼠进食量更多。在抑制LPA合成或敲除突触前LPA2受体后能够一定程度上抑制小鼠进食行为,减少体重。这些结果表明突触间脂质信号调控体重。
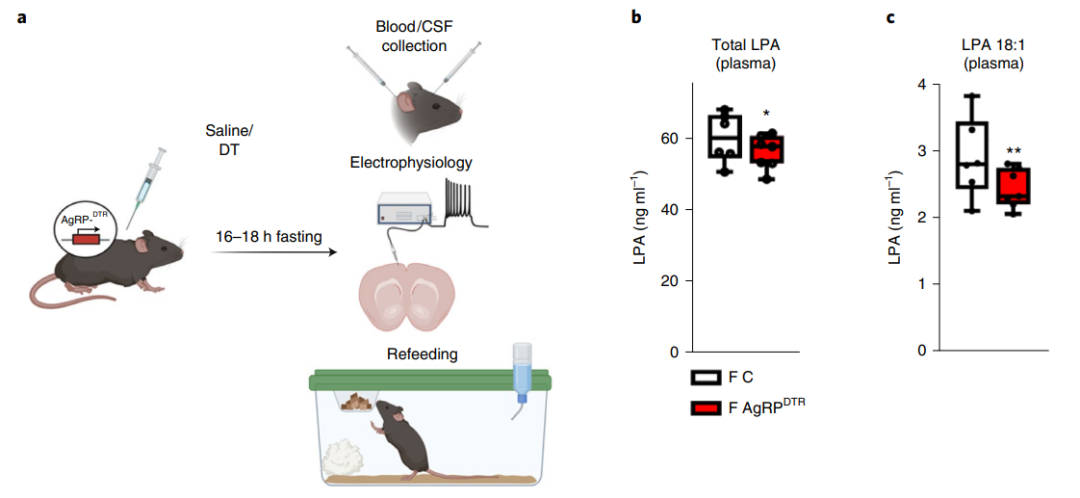
图3:抑制AgRP神经元后降低外周LPA水平
下丘脑弓状核内表达刺鼠相关肽(AgRP)的神经元参与禁食期间的外周脂质信号调节。激活AgRP神经元可促进食欲,减少能量代谢。
在特异性诱导AgRP神经元凋亡后禁食小鼠血清中LPA水平降低,皮层区域微小兴奋性突触后电流减弱,进食行为也明显减弱。这就表明外周来源的LPA可通过AgRP神经元实现调控摄食行为。
总的来说,本文揭示了外周能量变化(禁食)促进LPA合成,增强皮层区域神经元兴奋性,促进食欲,饮食增多,表明肝脏脂质信号可通过下丘脑实现调控摄食功能。
原始出处:
Jing Huang, et al. L-5-hydroxytryptophan promotes antitumor immunity by inhibiting PD-L1 inducible expression. Journal for immunotherapy of cancery, 2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#ERA#
43
#下丘脑#
46
#丘脑#
38
#丘脑#
54
认真学习~~
53