Neurosurgery:制定脑出血微创手术目标,以达到更佳疗效
2019-08-01 杨中华 脑血管病及重症文献导读
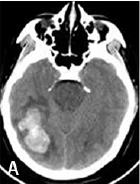
微创外科手术,包括立体定向导管rtPA溶解血凝块抽吸和清除血肿,是一项有希望的方法,以改善慕上脑出血的预后,降低致残率。最近发表了一项 III 期随机试验(MISTIE)发现这种方法能够降低死亡率,但是对主要终点未起到作用(1年 mRS 0-3)。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#surgery#
37
#GER#
30
#微创手术#
40
#微创#
32
#ROS#
32
谢谢梅斯提供这么好的信息,学到很多
50