J Thromb Haemost:COVID-19住院患者症状性静脉血栓栓塞临床特征和危险因素
2021-02-15 MedSci原创 MedSci原创
重症COVID-19患者具有较高的无症状静脉血栓栓塞(VTE)发生率,但一般COVID-19患者症状性VTE的特征尚未很好的归纳。近日,血栓和凝血疾病权威杂志Journal of Thrombosis
重症COVID-19患者具有较高的无症状静脉血栓栓塞(VTE)发生率,但一般COVID-19患者症状性VTE的特征尚未很好的归纳。近日,血栓和凝血疾病权威杂志Journal of Thrombosis and Haemostasis上发表了一篇研究文章,研究人员旨在全面探讨COVID-19患者VTE的患病率和风险预测。
这项回顾性研究纳入了2020年1月1日至3月31日在中国16个中心住院并发VTE的所有COVID-19患者。共有2779例患者被确诊为COVID-19。
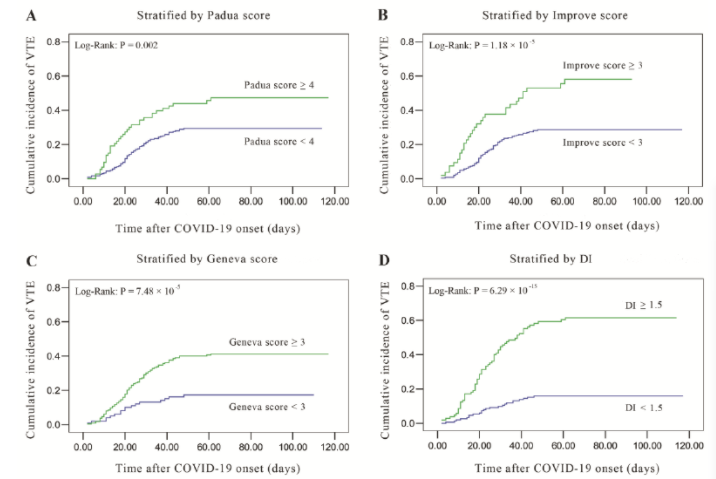
与23434名非COVID-19住院患者相比,重症和非重症COVID-19住院患者发生症状性VTE的ORs分别为5.94 (95%CI为3.91~10.09)和2.79 (95%CI为1.43~5.60)。当104例VTE患者和208例非VTE患者比较时,肺栓塞患者的住院死亡率更高(OR为6.74,95%CI为2.18~20.81)。在发病后平均21天发生VTE(IQR为13.25~31)。VTE的独立因素包括年龄增长、癌症、从症状开始到入院的时间间隔更长、入院时较低的纤维蛋白原和较高的D-二聚体水平、D-二聚体升高(DI)≥1.5倍;其中,DI≥1.5倍与之的相关性最为显著(OR为14.18, 95%CI为6.25~32.18,P=2.23×10‐10)。一种由3个简单的凝血变量(入院时纤维蛋白原、D-二聚体水平和DI≥1.5倍)组成的新预测模型对症状性VTE有良好的预测能力(AUC为0.865, 95%CI为0.822~0.907,敏感性为0.930,特异性为0.710)。
由此可见,COVID-19住院患者发生VTE的风险过高。新预测模型有助于早期识别VTE高危患者。
原始出处:
Jun‐Ying Li.et al.Clinical characteristics and risk factors for symptomatic venous thromboembolism in hospitalized COVID‐19 patients: A multicenter retrospective study.Journal of Thrombosis and Haemostasis.2021.https://doi.org/10.1111/jth.15261
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#临床特征#
30
#静脉血#
27
#HAE#
25
#静脉#
33
学习了
81