晚期肺结节病患者进行性纤维化间质性肺病表型的特征
2022-06-26 刘少飞 MedSci原创
严重受限的 DLCO 定义的晚期肺结节病患者队列的功能和放射学特征及预后。我们调查了有多少晚期肺结节病患者符合 PF-ILD 标准以及该亚组的预后。
晚期肺结节病会导致严重的发病率并可能导致死亡。大型试验证明了抗纤维化药物对进行性纤维化间质性肺病 (PF-ILD) 患者的疗效,包括一些结节病患者。迄今为止,对结节病中这种进行性纤维化表型知之甚少。一氧化碳弥散能力(DLCO)可能是筛查晚期肺结节病的有用功能标志物。在这项研究中,我们描述了一个患有晚期肺结节病的队列,并深入了解了结节病的进行性纤维化表型。
研究方法:
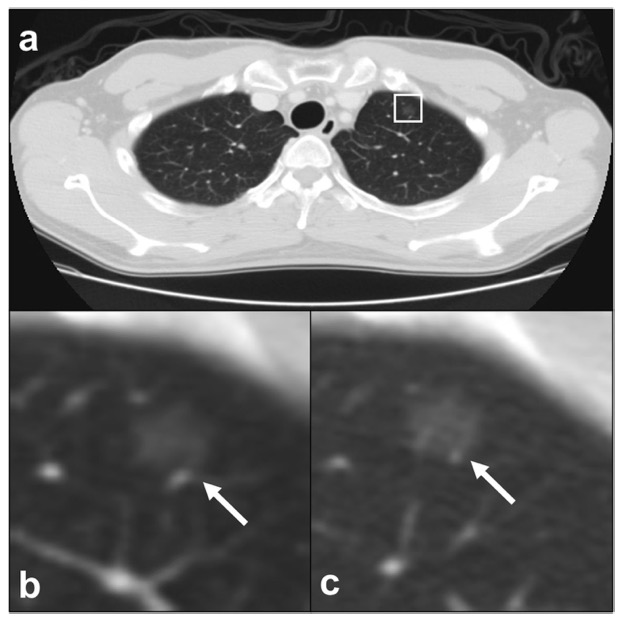
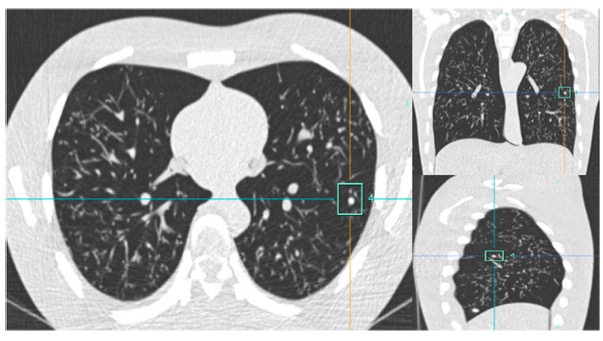
这项回顾性队列研究纳入了结节病和 DLCO < 50% 预测值的患者。DLCO < 50% 预测的第一次测量是基线。收集肺功能数据、HRCT、肺动脉高压(PH)和死亡率。HRCT 上纤维化 > 10% 的患者符合 24 个月内 ILD 进展的标准被标记为 PF-ILD。用 Cox 回归分析建立了死亡率的预测因子。
研究结果:
包括 106 名 DLCO < 50% 预测值的患者。随访 2 年后,患者用力肺活量 (FVC) 的变化幅度很大,从 - 34% 到 + 45%,而 DLCO 的变化在 - 11% 和 + 26% 之间。14 名患者(15%)符合 PF-ILD 标准,其中 6 名(43%)在 10 年内死亡,而非 PF-ILD 组有 10 名(13%)(p = 0.006)。PH 存在 12 (11%)、56 (53%) 在 HRCT 上显示 > 10% 的纤维化。整个队列中死亡率和肺移植的独立预测因子是 PH、PF-ILD 和 UIP 样模式。
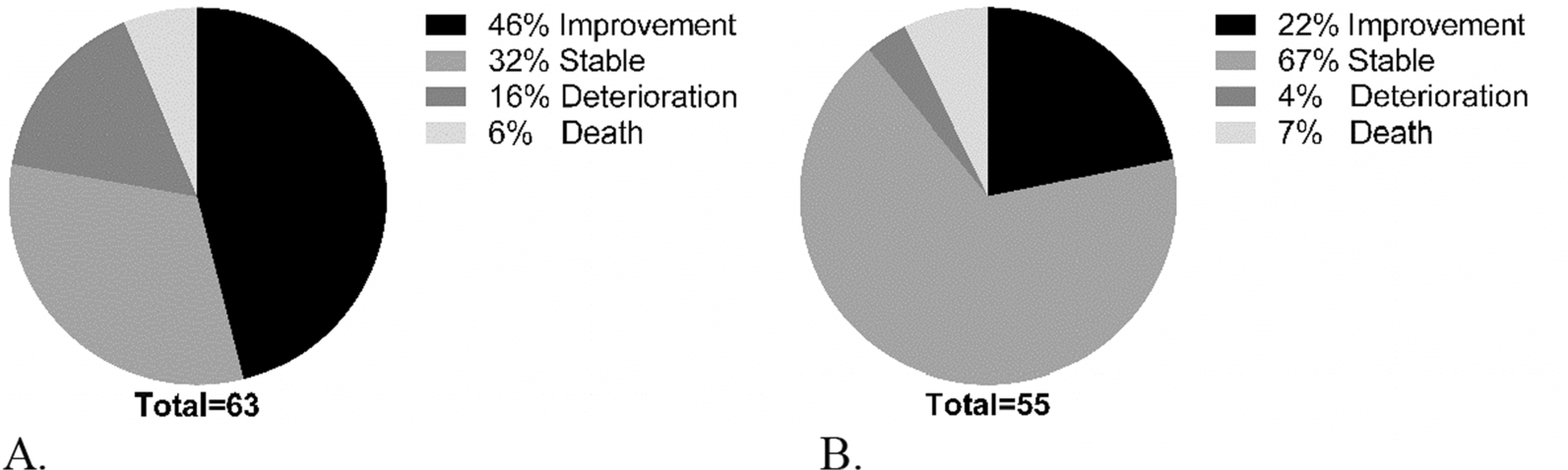
肺功能改善、稳定或恶化的患者与死亡患者的比例。
研究结论:
这项基于弥散能力严重受损的晚期肺结节病患者的研究中,我们证明 15% 的患者符合当前进行性纤维化 ILD (PF-ILD) 的标准。在我们的研究队列中,我们发现 HRCT 上的 PH、PF-ILD 和 UIP 样模式是全因死亡率和肺移植的独立预测因子。在符合 PF-ILD 标准的结节病组中,43% 的患者死亡或接受了双侧肺移植,而非 PF-ILD 的总死亡率为 13%。总之,在这一组中,晚期肺结节病的病程变化很大,从功能显着改善到死亡。PF-ILD 患者的死亡率高于整个肺结节病组的死亡率。未来的研究应集中在这些患者中添加抗纤维化药物。
参考文献:
Schimmelpennink MC, Meek DB, Vorselaars ADM, Langezaal LCM, van Moorsel CHM, van der Vis JJ, Veltkamp M, Grutters JC. Characterization of the PF-ILD phenotype in patients with advanced pulmonary sarcoidosis. Respir Res. 2022 Jun 25;23(1):169. doi: 10.1186/s12931-022-02094-7. PMID: 35752806.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#间质性#
51
#进行性纤维化#
41
#进行性#
52
#纤维化间质性肺病#
53
#肺病#
50
#表型#
36