Neurology:误诊为脑静脉窦血栓形成的先天性变异:临床陷阱
2019-05-27 zyx整理 神经科病例撷英拾粹
23岁女性,罹患脑静脉窦血栓形成(CVST)服用华法林治疗,表现为急性化脓性关节血肿,需要手术治疗。
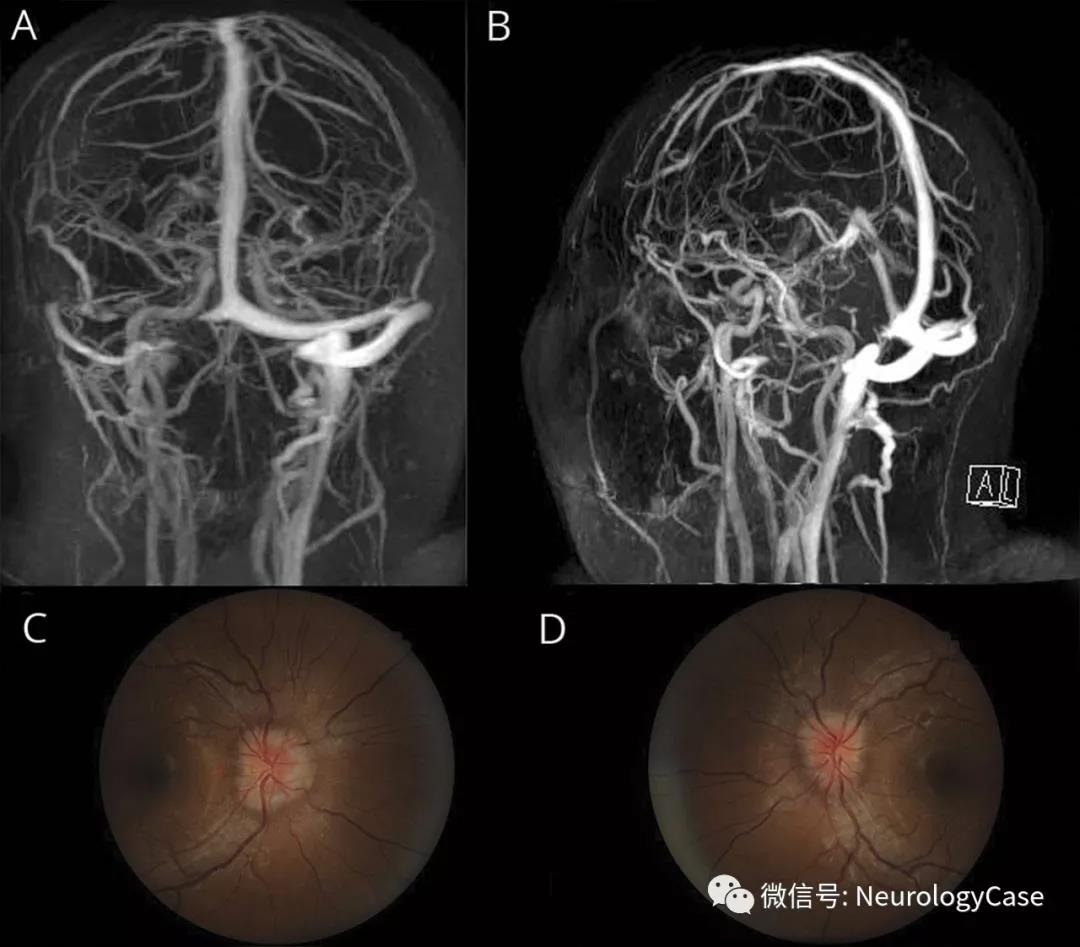
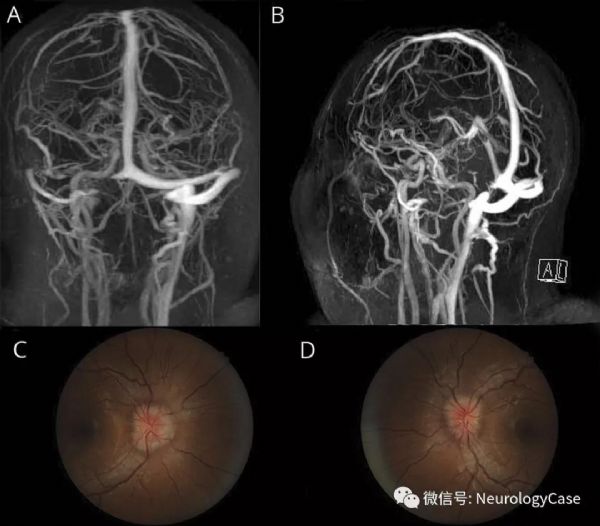
23岁女性,罹患脑静脉窦血栓形成(CVST)服用华法林治疗,表现为急性化脓性关节血肿,需要手术治疗。为抗凝治疗建议进行脑血管相关咨询。脑磁共振静脉造影显示右侧横窦发育不全(图)。停用抗凝治疗。鉴于患者有头痛和视乳头水肿病史,临床怀疑特发性颅内高压(IIH),开始给予乙酰唑胺治疗。
单侧横窦发育不全是一种正常变异,见于20%-39%的健康人,且可貌似CVST。IIH的横窦狭窄也可貌似CVST。上述情况误诊为CVST可导致严重的并发症。
(图:A-B:磁共振静脉造影提示右内侧横窦发育不全,可能是先天性变异;在Labbe静脉侧面,右侧横窦和乙状窦很小;左侧横窦,上矢状窦,大脑内静脉和直窦外观基本正常;C:右侧眼底照相提示2级视乳头水肿[Frisen分级量表];D:左侧眼底照相提示2级视乳头水肿)
原始出处:Dawit S, Das DM, Acierno MD, O'Carroll CB. Teaching NeuroImages: Congenital variant misdiagnosed as cerebral venous sinus thrombosis: Clinical pitfall. Neurology. 2019 Apr 23;
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#静脉#
36
#静脉窦血栓#
48
#Neurol#
35
#变异#
38
#先天性#
31
#静脉窦#
29