Eur Ann Allergy Clin Immunol:过敏性结膜炎的严重程度和持续时间与过敏性鼻炎和哮喘的严重程度和持续时间有关吗?
2021-08-15 AlexYang MedSci原创
过敏性结膜炎(AC)是一种由免疫球蛋白(Ig)E超敏反应介导的结膜炎症反应。根据不同的地理区域和研究设计,AC在普通人群中的估计患病率在15-40%之间。
过敏性结膜炎(AC)是一种由免疫球蛋白(Ig)E超敏反应介导的结膜炎症反应。根据不同的地理区域和研究设计,AC在普通人群中的估计患病率在15-40%之间。

目前为止,人们对过敏性结膜炎(AC)与鼻炎和/或哮喘的关系了解甚少。

近期,有研究人员将过敏性结膜炎共识文件(DECA)的标准应用于过敏性结膜炎患者群体的分类,以评估过敏性结膜炎的严重程度和持续时间与鼻炎和/或哮喘的关系。
研究纳入了参加 "2015年过敏性疾病研究 "的有眼部症状的AC患者。研究人员按年龄组(小于或等于14岁和大于14岁)对人口统计学、根据DECA标准的分类、病因和合并症进行了评估。
研究共有2914名患者(年龄范围为1-90岁)纳入 了"Alergológica 2015 "研究中。其中,965名患者(33.1%)诊断为AC(77.5%大于14岁)。按照疾病的严重程度,分别有1.8%、46.4%和51.8%的AC分为重度、中度或轻度;按照疾病的持续时间,分别有51.6%和48.4%的患者分为间歇性或持续性。有4%的病人只患有AC。AC主要与鼻炎(88.4%)、哮喘(38.2%)、食物过敏(8.3%)和特应性皮炎(3.5%)有关。在过敏性呼吸道疾病中,鼻炎先于AC发生,而哮喘则后于AC发生。AC的严重程度和持续时间与鼻炎(两个年龄组的P<0.001)和哮喘(仅成人的P<0.001)的严重程度和持续时间有显著关系。

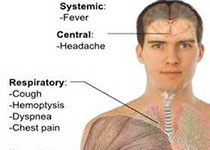
AC与鼻炎或哮喘之间的相关性
综上所述,使用新DECA标准对AC分类表明AC、鼻炎和哮喘的严重程度和持续时间之间存在直接关系。这些关系表明,AC应该认为是 "同一气道,同一疾病 "假说的一个组成部分。
原始出处:
M C Sánchez-Hernández , M T Dordal , A M Navarro et al. Severity and duration of allergic conjunctivitis: are they associated with severity and duration of allergic rhinitis and asthma? Eur Ann Allergy Clin Immunol. Jul 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#过敏性结膜炎#
44
#结膜炎#
64
#过敏性#
47
#ALL#
45
#持续时间#
51