Blood:树突细胞来源的IL-6失调介导alloSCT后移植物抗宿主病的发生
2020-01-02 不详 MedSci原创
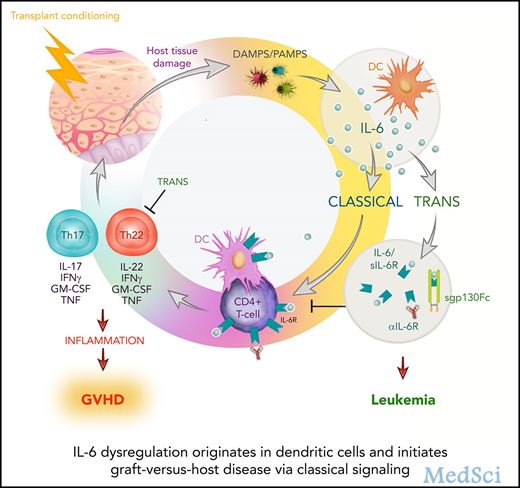
中心点:DCs是异体移植后IL-6失调的主要来源。IL-6依赖性GVHD受供体T细胞上的IL-6R经典信号驱动,但受反式信号调控。摘要:异体干细胞移植(alloSCT)后移植物抗宿主病(GVHD)的特点是白细胞介素-6 (IL-6)调节异常。IL-6可以通过多种途径介导作用,包括经典、反式和簇信号。鉴于近年来有多种药物可以抑制这些离散的信号级联,了解细胞因子的来源、信号和细胞靶点对临床研究的设计至
DCs是异体移植后IL-6失调的主要来源。
IL-6依赖性GVHD受供体T细胞上的IL-6R经典信号驱动,但受反式信号调控。
摘要:
异体干细胞移植(alloSCT)后移植物抗宿主病(GVHD)的特点是白细胞介素-6 (IL-6)调节异常。IL-6可以通过多种途径介导作用,包括经典、反式和簇信号。鉴于近年来有多种药物可以抑制这些离散的信号级联,了解细胞因子的来源、信号和细胞靶点对临床研究的设计至关重要。
在本研究中,研究人员发现受体树突细胞(DCs)分泌的IL-6可引发这种细胞因子的系统性失调。在T细胞中,通过靶向敲除IL-6受体(IL-6R)抑制DC驱动的经典信号可消除致病性供体Th17/Th22细胞分化,进而获得长期存活。移植后,供体DCs承担同样的角色,维持经典IL-6信号依赖性GVHD反应。
意外的是,移植后的集束信号并不活跃,而用可溶性gp130Fc抑制反式信号可促进严重的、慢性皮肤GVHD的发生。后者是多功能性Th22细胞过度增殖的结果,IL-22缺失或IL-6R抑制可逆转这一结果。重要的是,抑制IL-6经典信号并不影响移植物抗白血病的效果。
总而言之,本研究结果强调了IL-6信号和下游Th17/Th22分化可作为alloSCT后的重要治疗靶点。
原始出处:
Andrew N. Wilkinson, et al.IL-6 dysregulation originates in dendritic cells and mediates graft-versus-host disease via classical signaling.Blood. December 5, 2019.
本文系梅斯医学(MedSci)原创编译,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#树突细胞#
42
#植物#
32
#IL-6#
40
#ALL#
26
#宿主#
27
#移植物抗宿主病#
34
#移植物#
31