Breast Cancer Research:PM2.5增加女性患乳腺癌的风险
2017-04-07 浮生若梦 来宝网
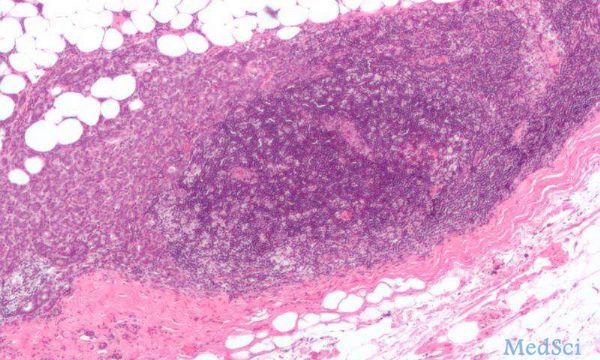
根据开放获取期刊《乳腺癌研究》上发表的最新研究显示,在美国,一项近28万妇女参与的调查发现,生活在空气污染细颗粒物水平较高的地区可能增加女性的乳房密度-这是乳腺癌确定的风险因素之一。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#AST#
31
认真学习,把间接经验应用到临床实践中去,然后再总结出新思路。
82
#PM2.5#
44
#Breast#
37
#Research#
30
学习了,谢谢!
72
PM2.5增加女性患乳腺癌的风险
73