Lancet Oncol:普拉替尼有望用于治疗RET融合阳性的非小细胞肺癌(ARROW试验)
2021-06-26 MedSci原创 MedSci原创
RET的致癌改变已在多种肿瘤类型中被发现,包括1-2%的非小细胞肺癌(NSCLC)。我们旨在评估帕拉西替尼的安全性、耐受性和抗肿瘤活性,帕拉西替尼是一种强效口服选择性RET抑制剂,用于RET融合阳性N
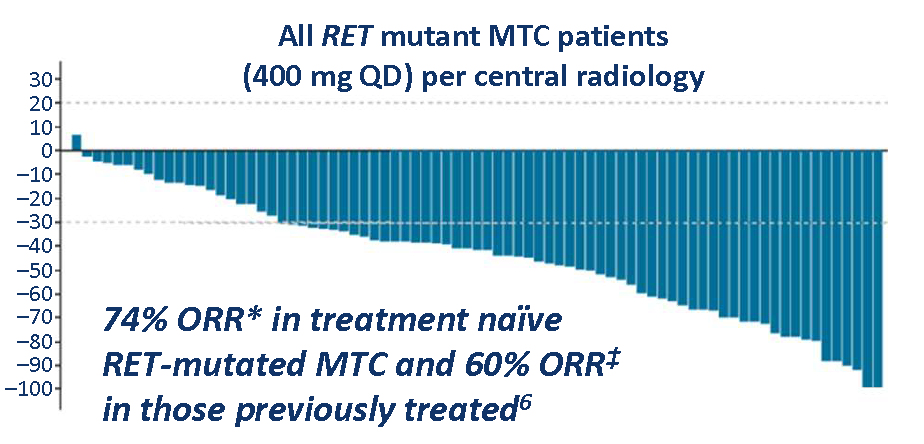
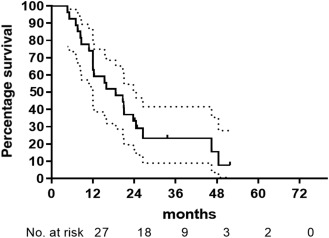
RET的致癌改变已在多种肿瘤类型中被发现,包括1-2%的非小细胞肺癌(NSCLC)。我们旨在评估帕拉西替尼的安全性、耐受性和抗肿瘤活性,帕拉西替尼是一种强效口服选择性RET抑制剂,用于RET融合阳性NSCLC患者。 本研究旨在评估普拉替尼(Pralsetinib,一种高效、口服、选择性 的RET抑制剂)用于RET融合阳性NSCLC患者的安全性、耐受性和抗肿瘤活性。 ARROW试验是一项在12个国家的71个地点开展的多队列、开放标签的1/2期研究,招募了年满18岁的局部晚期或转移性实体瘤患者,包括携带RET融合阳性的NSCLC患者。纳入年龄在18岁或以上的局部晚期或转移性实体肿瘤患者,包括RET融合阳性NSCLC,以及东部肿瘤合作组(Eastern Cooperative Oncology Group) 0-2的表现状态(后来在协议修订中限制为0-1)在2期阶段,患者每日口服400 mg的普拉替尼治疗,直到病情进展、不耐受、撤出试验或调查员决定。主要终点是总缓解率(根据实体肿瘤反应评价标准1·1版本,并通过盲法独立中心评审进行评估)和安全性。对RET融合阳性NSCLC患者的肿瘤反应进行评
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Oncol#
35
#Lancet#
0
#RET#
48
#非小细胞#
45
#融合#
50
顶刊就是不一样,质量很高,内容精彩!学到很多
53
谢谢梅斯分享这么多精彩信息
44