J Periodontol:正畸关闭拔牙间隙的时间点是否影响牙龈裂的发生率?
2020-05-31 网络 网络
在正畸关闭拔牙间隙的过程中经常会出现牙龈裂(GC),可能会影响治疗效果。本研究评估了在拔牙后,正畸关闭拔牙间隙的时间点对GC发生的影响。
在正畸关闭拔牙间隙的过程中经常会出现牙龈裂(GC),可能会影响治疗效果。本研究评估了在拔牙后,正畸关闭拔牙间隙的时间点对GC发生的影响。
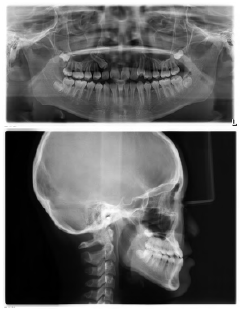
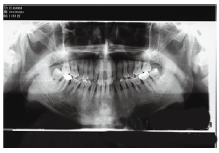
实验纳入25名患者,因正畸需要拔除双侧前磨牙,随机选择一个前牙,拔除后8周行正畸关闭间隙("延迟移动,"DM),而对侧前牙在拔除1周后正畸("早期移动,"EM,"治疗组")。在3个月和6个月后("时间点")检测GC的存在或不存在,并评估与各种参数(即治疗组、时间点、性别、颌骨、颅面生长、牙龈生物型、拔牙后颊侧牙槽骨开裂、间隙关闭)的关系。
最终共有21名患者的26个病例被纳入分析。在3个月后(DM:53.9%;EM:69.2%)和6个月后(DM:76.9%;EM:88.5%)GC发生率很高。EM(P = 0.014)和较大的间隙关闭(P = 0.001)导致GC的发生率显着升高。此外,在颊侧牙槽骨开裂(P = 0.052)和牙龈薄扇型(P = 0.054)的病例中,GC的发生也会增加。"快速移动"(这里指的是每月牙齿移动≥1 mm的病例)在3个月后有>90%的病例发生GC。"慢速移动 "在3个月和最终评估中,分别有25%和70%的病例发生GC。
GC是正畸关闭拔牙间隙过程中经常发现的一种现象,而且似乎在牙齿移动早期时和 "快速移动 "中更容易发生。
原文出处:
Kristina Bertl,Does the time‐point of orthodontic space closure initiation after tooth extraction affect the incidence of gingival cleft development? A randomized controlled clinical trial, journal of periodontology, 2020 May,doi.:10.1002/JPER.19-0376
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#发生率#
33
#PE#
36
#正畸#
33
#拔牙#
36