JNCCN:免疫治疗相关食管炎的临床特征、治疗反应和预后
2021-06-13 yd2015 MedSci原创
免疫治疗相关性食管炎的发生率较低,大多为轻度症状,并且使用非免疫抑制治疗方法可控制,类固醇激素的使用效果不明确。因此,仍需要长时间随访的大型前瞻性研究来评估。
免疫检查点抑制剂(ICIs)越来越常用于肿瘤治疗,并且展示出良好的抗肿瘤疗效。常用的ICIs有CTLA4、PD1和PDL1抑制剂。免疫治疗相关不良反应也是临床上值得关注的问题。免疫相关胃肠道反应因为不常见而没有得到很好的了解。因此,来自美国德克萨斯大学MD安德森癌症中心的研究团队开展了一项回顾性研究,评估免疫相关食管炎的临床特征、治疗反应和预后。相关成果发表在Journal of the National Comprehensive Cancer Network(JNCCN)杂志上。

该研究是回顾性研究,纳入MD安德森癌症中心2011年6月至2020年1月接受ICIs治疗的657例患者。在ICIs治疗期间或治疗后6月内接受食管胃镜检查,发现21例患者(3%)出现免疫相关食管炎。其中1例(5%)单独接受CTLA-4抑制剂治疗,15例(71%)接受抗PD -1或PD-L1单药治疗,5例(24%)接受联合治疗。4例(19%)患者接受联合化疗,比如常见的培美曲塞,多西他赛和阿糖胞苷。只有1例(5%)患者在免疫相关食管炎出现前3个月内服用过NSAIDs。最常见的恶性肿瘤为非小细胞肺癌 (n=6; 29%), 胃肠道肿瘤(n=4; 19%) 和黑色素瘤(n=4; 19%)。
最常见的EGD检查原因为恶心呕吐(33%),吞咽困难(19%),或呕血(19%)。从ICIs治疗开始至免疫相关食管炎出现的中位时间为4个月(2–9个月),中位免疫相关食管炎症状持续时间为30天(IQR, 9–43天)。大部分患者(n=17; 81%) 为轻度的食管炎(CTCAE grade 1–2)。

临床症状
内镜和组织学特征发现,经EGD评估,只有3例患者(14%)单纯性食管受累,18例患者(86%)并发累及胃、十二指肠或两者。共有11例(52%)患者有食管多段炎症,而其他患者有食管中段三分之一的孤立累及(n=7;33%),食管远端三分之一(n=2;10%),或胃食管交界处(n=1;5%)。只有10名患者(48%)接受了食管活检,其中5例为急性炎症,5例为慢性炎症。
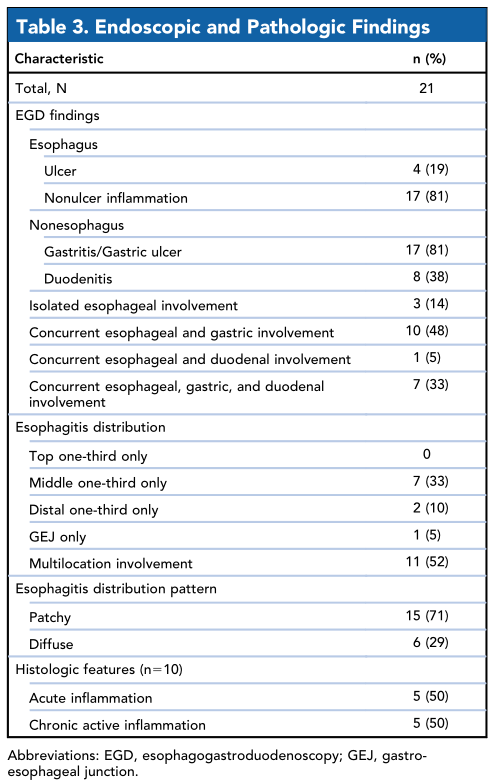
内镜和组织学特征
共有10例(48%)患者因上消化道症状需要住院治疗。患者最多接受的是PPI治疗(n=14;67%);只有4例(19%)使用类固醇(3例使用强的松,1例使用口服布地奈德),中位持续时间为50天(IQR, 35-134天)。免疫相关食管炎引起的严重并发症比较少见,3例(14%)患者在EGD时出血,1例(5%)需要全肠外营养支持。15例患者因为所有的免疫相关不良反应而永久停止了ICIs的治疗。只有2例患者因为食管炎是主要的毒性作用而导致ICIs的中断治疗。研究期间8例(38%)患者死亡(中位随访,15个月[IQR, 4个月至4.2年]),死因为患者的恶性肿瘤引起。

食管炎治疗转归
研究者比较了除使用ICIs外患者存在食管炎危险因素和无危险因素的临床特点。危险因素定义为食管炎发病前3个月内使用非甾体抗炎药,食管炎发病前3个月内进行化疗,以及ICIs治疗时同时联合化疗。两组患者的炎症特征(P=0.92)、食管炎分布(P=0.36)、从开始使用ICI到食管炎发病的时间(P=0.34)、住院时间(P=0.71),或症状(P=0.77)均无统计学差异。

食管炎危险因素
综上,免疫治疗相关性食管炎的发生率较低,大多为轻度症状,并且使用非免疫抑制治疗方法可控制,类固醇激素的使用效果不明确。因此,仍需要长时间随访的大型前瞻性研究来评估。
原始出处:
Kavea Panneerselvam, Rajan N. Amin, Dongguang Wei,et al. Clinicopathologic Features, Treatment Response, and Outcomes of Immune Checkpoint Inhibitor-Related Esophagitis. J Natl Compr Canc Netw. doi: 10.6004/jnccn.2020.7675. Published online June 11, 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#临床特征#
35
#NCCN#
0
#食管#
27
#食管炎#
42
十分有帮助
48
ICI相关食管炎
48