Sci Transl Med:重磅疗法治疗脑瘤,研究展现曙光
2017-07-21 佚名 学术经纬
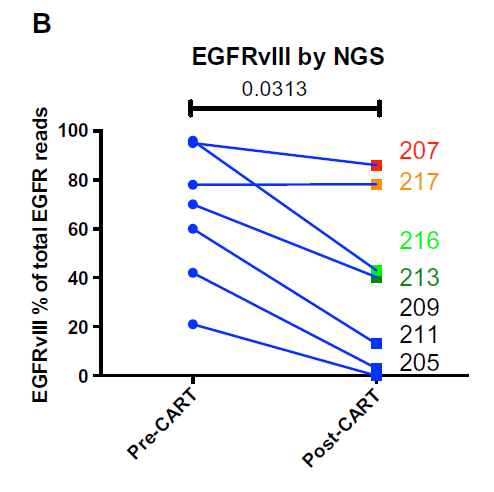
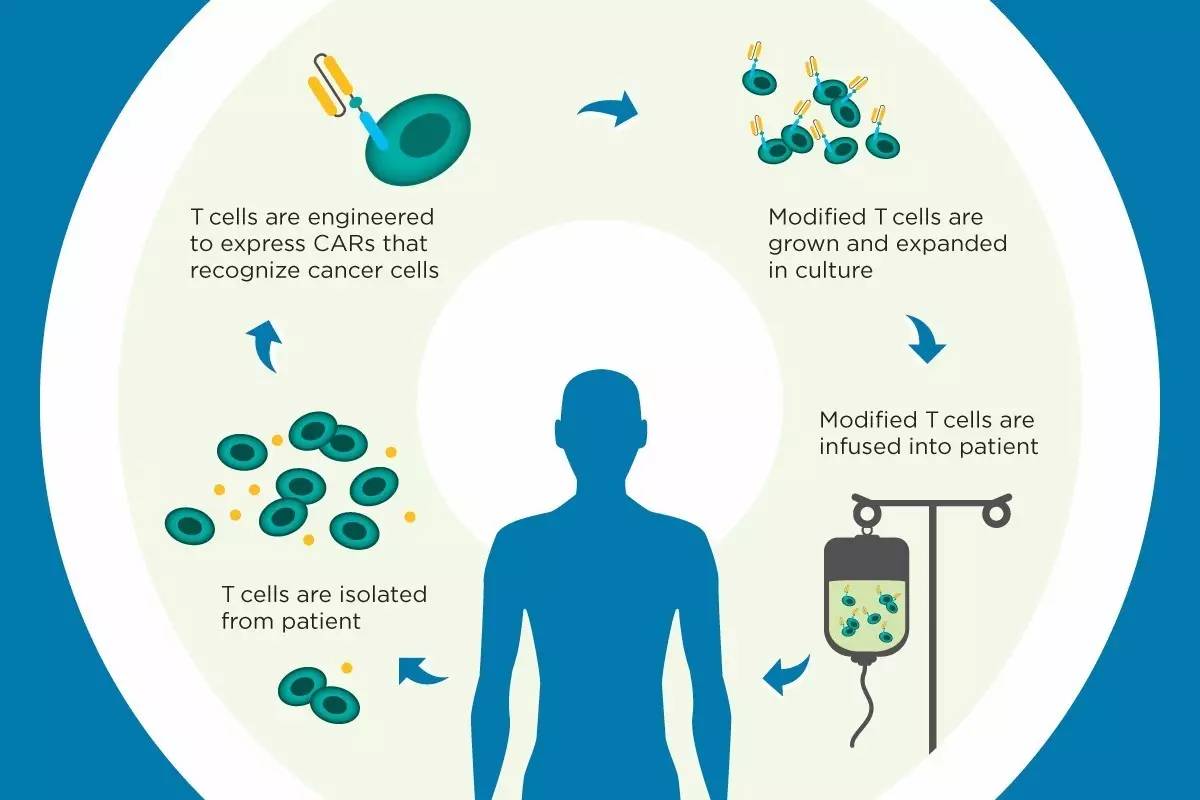
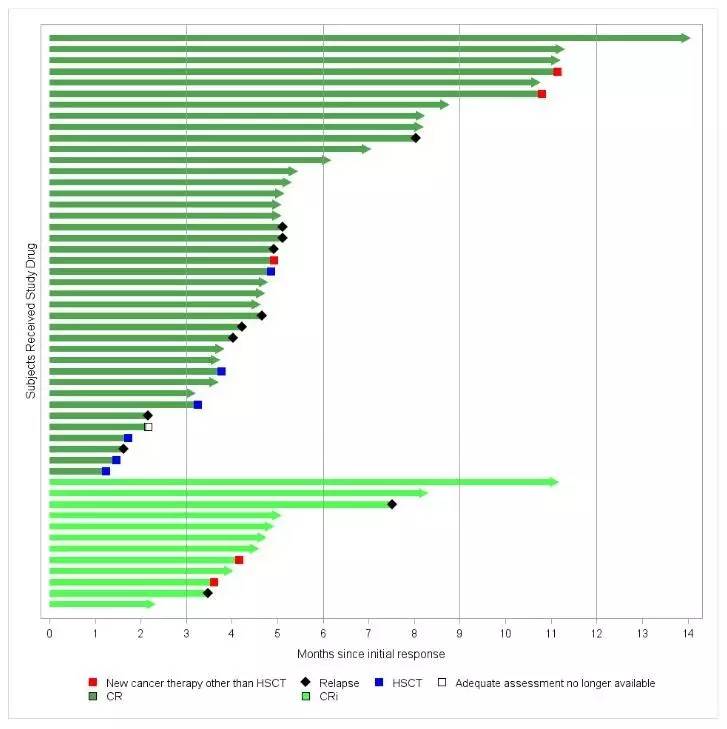
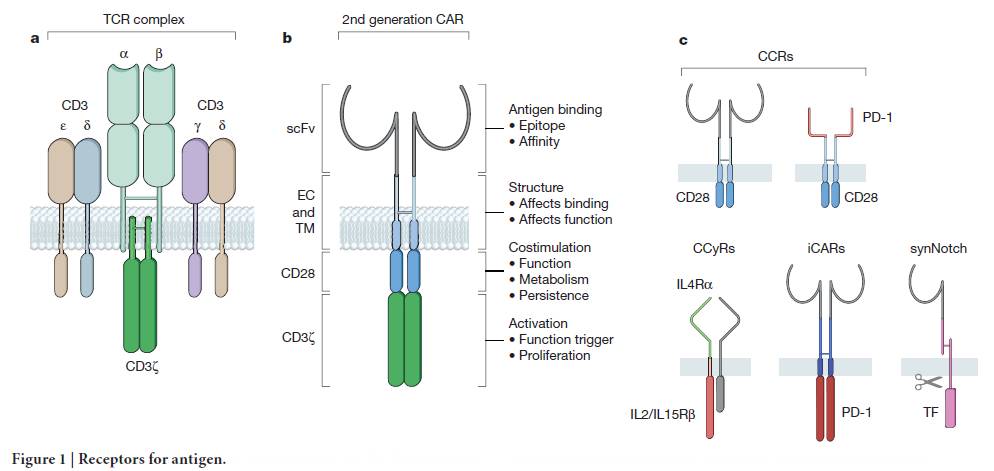
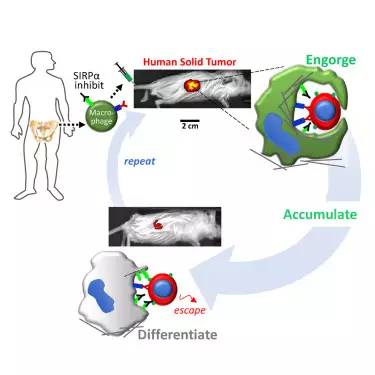
在一项临床试验中,研究人员们招募了一批表达EGFRvIII,且病情出现复发的胶质母细胞瘤患者。利用这些患者体内的T细胞,研究人员开发出了CAR-T-EGFRvIII疗法,特异性地针对患者的癌细胞。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Transl#
24
#曙光#
32
#TRA#
28
#脑瘤#
30
#重磅#
31
#Med#
19
学习,谢谢分享
70