Lancet Oncol:来曲唑延长治疗5年可显著提高已绝经的早期乳腺癌患者的生存预后
2021-09-18 Nebula MedSci原创
来曲唑延长治疗5年可相比来曲唑标准治疗2-3年显著提高既往接受过他莫西芬治疗2-3年的已绝经的乳腺癌患者的无病生存率
芳香化酶抑制剂是目前临床广泛应用于绝经后乳腺癌的一类内分泌治疗的药物。在既往使用过芳香化酶抑制剂的情况下,延长芳香化酶抑制剂治疗时间超过 5 年的益处仍存在争议。
本研究旨在对比芳香化酶抑制剂来曲唑延长疗法(5年)对比来曲唑标准疗法(2-3年)用于已经接受他莫昔芬治疗2-3年的绝经后的乳腺癌患者中的效益和安全性。
这是一项在意大利的69家医院开展的多中心、开放标签、随机的3期试验,招募了已绝经的、组织学确诊的I-III期的、可手术治疗的侵袭性激素受体阳性的乳腺癌患者,且要求既往接受他莫西芬辅助治疗满两年且不超过3年3个月、无复发迹象、ECOG表现状态≤2分。受试患者被随机(1:1)分至对照组(来曲唑治疗2-3年)和延长组(来曲唑治疗5年),每日口服来曲唑 2.5 mg。主要终点是无侵袭性疾病生存率。
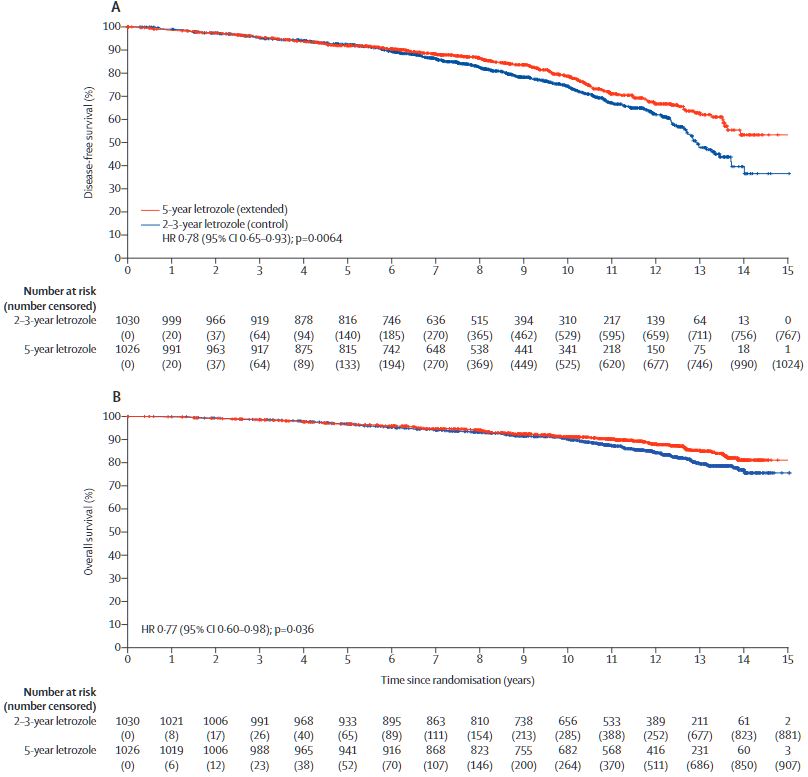
两组的无病生存率和总生存率
2005年8月1日至2010年19月24日,共招募了2056位患者,随机分至对照组(n=1030)和延长组(n=1026)。中位随访了11.7年(范围 9.5-13.1年)后,对照组和延长组分别有262位(25.4%)和212位(20.7%)患者获得了无病生存事件。对照组和延长组的12年无病生存率分别是 62%(95% CI 57-66)和67%(62-71)(风险比 0.78, 95% CI 0.65-0.93; p=0.0064)。
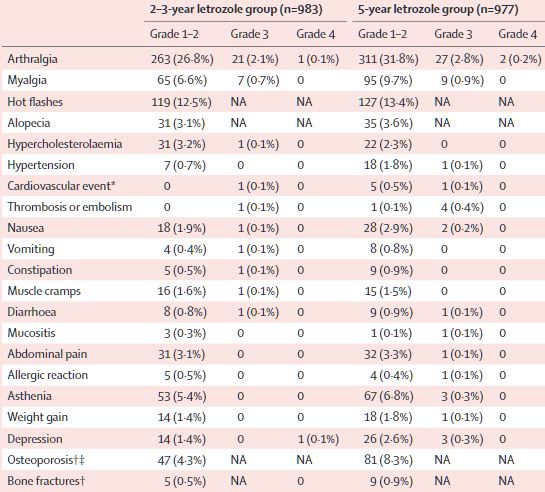
不良事件
最常见的3级或4级不良事件有关节痛(对照组 vs 延长组:2.2% vs 3.0%)和肌痛(0.7% vs 0.9%)。对照组发生了3例(0.3%)严重的治疗相关的不良事件,延长组发生了8例(0.8%)。未观察到毒性作用导致的死亡事件。
总而言之,来曲唑延长治疗5年可相比来曲唑标准治疗2-3年显著提高既往接受过他莫西芬治疗2-3年的已绝经的乳腺癌患者的无病生存率。他莫西芬内分泌治疗2-3年,继以来曲唑治疗5年的序贯疗法,或可作为已绝经的激素受体阳性的乳腺癌患者的最佳标准内分泌治疗方法之一。
原始出处:
Lucia Del Mastro, et al. Extended therapy with letrozole as adjuvant treatment of postmenopausal patients with early-stage breast cancer: a multicentre, open-label, randomised, phase 3 trial. The Lancet Oncology. September 17, 2021. https://doi.org/10.1016/S1470-2045(21)00352-1
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#Lancet#
28
#Oncol#
24
#生存预后#
27
#绝经#
33
#来曲唑#
50
#乳腺癌患者#
31
学习
43