NEJM:BIVV001可维持严重A型血友病患者长期较高水平的VIII因子活性
2020-09-10 MedSci原创 MedSci原创
对于严重A型血友病患者,单次静脉注射BIVV001可维持长时间较高水平的VIII因子活性,半衰期是重组VIII因子的4倍,且安全性良好
VIII因子替代物极大程度上改善了A型血友病患者的病情,但大多数替代物的半衰期较短,极大限制了其临床应用,虽然重组VIII因子产品的半衰期可提高至15-19小时,但仍需要更为有效的提高VIII因子半衰期方法。 BIVV001(rFVIIIFc-VWF-XTEN)是一种新型的融合蛋白,近日研究人员考察了单剂量BIVV001治疗的安全性和药代动力学数据。

本次研究为1-2a期试验中, 16名男性(18-65岁)严重A型血友病(因子VIII活性<1%)患者接受单次静脉注射重组VIII因子,剂量为每公斤体重25 IU(低剂量组)或65 IU/kg(高剂量组),注射后至少间隔3天,然后,患者接受单次静脉注射BIVV001,相应剂量为每公斤25 IU或65 IU。研究的主要终点为不良事件和药代动力学数据。

BIVV001结构及给药方案
单剂量BIVV001注射后28天,未检测到其对VIII因子抑制作用,也未发生过敏事件。 BIVV001的几何平均半衰期是重组VIII因子的3至4倍(低剂量组:37.6 vs 9.1小时,高剂量组:42.5 vs 13.2小时)。两个BIVV001剂量组的VIII因子曲线下面积(AUC)是重组VIII因子的6到7倍(低剂量组:4470 vs 638小时×IU每分升,高剂量组:12800 vs 1960小时×IU每分升)。高剂量BIVV001注射后,患者第4天VIII因子的平均水平达到正常范围(≥51%),第7天为17%,这表明BIVV001治疗可以实现周间隔给药。
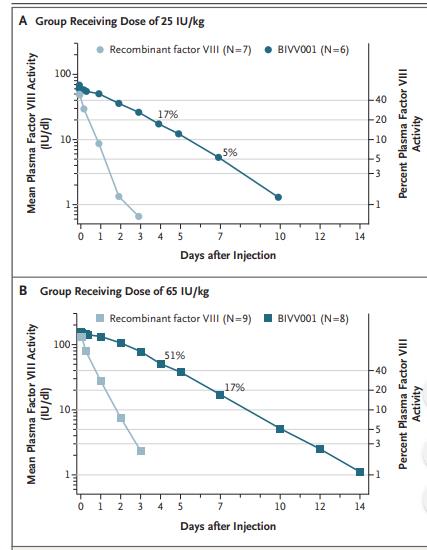
组间VIII因子活性差异
对于严重A型血友病患者,单次静脉注射BIVV001可维持长时间较高水平的VIII因子活性,半衰期是重组VIII因子的4倍,且安全性良好。
原始出处:
Barbara A. Konkle et al. BIVV001 Fusion Protein as Factor VIII Replacement Therapy for Hemophilia A. N Engl J Med, September 10, 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#BIVV001#
38
#A型血#
32
#III#
34
#VIII因子#
40
好
90
#A型血友病#
32
正在学习中
95
高水平文章
99
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
65
学习
91