OCC 2020:苏晞:心房颤动患者血栓整体管理的目标和决策
2020-06-02 门诊新视野 《门诊》杂志
房颤患者的抗栓治疗历来是一个值得关注的话题,房颤患者经过有效的抗栓管理后可以显著改善预后,提高患者的生活质量。但不同情况下的房颤患者的抗栓策略有所不同,面对纷繁复杂的临床病例,如何选择和调整策略是所有
房颤患者的抗栓治疗历来是一个值得关注的话题,房颤患者经过有效的抗栓管理后可以显著改善预后,提高患者的生活质量。但不同情况下的房颤患者的抗栓策略有所不同,面对纷繁复杂的临床病例,如何选择和调整策略是所有临床医师面对的共同挑战。2020年5月29日,在“第十四届东方心脏病学会议(OCC 2020)”血栓相关疾病专场上,来自武汉亚洲心脏病医院的苏晞教授从多角度分析,围绕房颤患者的抗栓决策进行了详细阐述。 房颤患者血栓管理的重要性 有临床数据显示,卒中在我国疾病死亡原因中占首位,而近50%心源性卒中的发生由房颤导致。大量循证研究证明,与非房颤患者相比,房颤相关卒中临床预后更差,严重残疾、死亡率、复发率都会显著增加。为此,国务院发布的《健康中国行动(2019-2030年)》文件中,将房颤患者的防控与管理也纳入其中,并建议房颤患者需遵医嘱采用抗凝治疗。 房颤患者血栓整体管理概览 欧美指南也对房颤患者NOAC的临床应用都有所推荐。2016年欧洲房颤指南明确指出:CHA2DA2-VASc评分≥2分的患者优先选择NOAC。2019年AHA/ACC/HRS房颤管理指南也明确推荐,对NOAC适用的房颤患者(除外中到重度二尖瓣狭窄或机械心脏瓣膜),与华法林相比更推荐使用NOAC(Ⅰ类推荐,A级证据);除中-重度二尖瓣狭窄、心脏机械瓣膜之外的房颤患者,如果使用华法林但不能保持治疗窗的INR值,建议使用NOAC(Ⅰ类推荐,C-EO级证据)。 不同情况下房颤患者血栓预防结果
接受PCI治疗的房颤患者需接受口服抗凝药联合DAPT的三联抗栓治疗,以降低心源性血栓和支架内血栓的发生风险。对此,北美和欧洲的专家共识有不同的推荐(图1)。北美专家共识推荐,房颤行PCI术后高缺血风险患者三联治疗(OAC+DAPT)1个月后可转为双联治疗(OAC+SAPT)12个月;房颤行PCI术后高出血风险患者双联治疗(OAC+SAPT)6个月后转为口服抗凝药;欧美专家共识推荐房颤行PCI术后高缺血风险患者三联治疗延长至6个月;房颤行PCI术后极高出血风险患者可双联治疗至12个月。
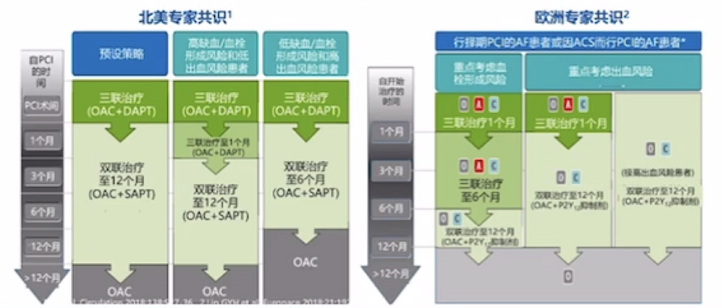
图1. 北美和欧洲专家共识推荐
房颤行左心耳封堵术患者
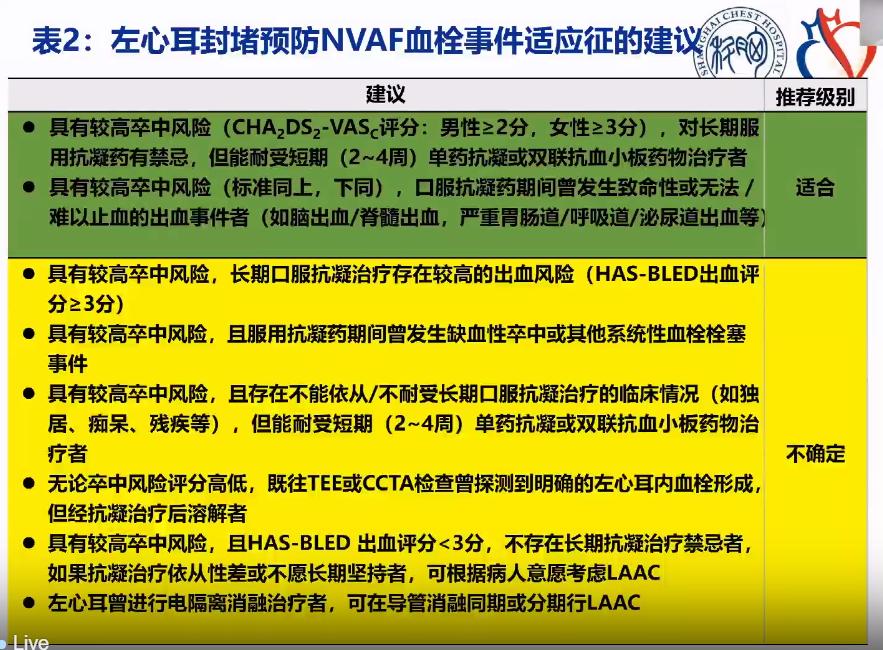
左心耳封堵术(LAAC)是预防房颤卒中的有效方法。2016年ESC和2019年ACC/AHA房颤管理指南均推荐:有长期口服抗凝药禁忌证的房颤患者,可以考虑左心耳封堵术(Ⅱb,B)。LAAC术后有抗凝治疗的阶段,但目前暂无统一的方案,临床医生需根据患者的出血和栓塞风险再来判定。
总 结
卒中已成为我国疾病死亡的首位病因,房颤的血栓管理至关重要。抗凝是房颤患者血栓管理中的重要治疗策略,大量循证医学证据已证实,NOAC的抗凝疗效优于传统的华法林。但临床医师在面对不同情形下的房颤患者,仍应根据血栓形成特点和风险进行血栓管理。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















学习了
68
#OCC#
46
#OCC 2020#
32
#决策#
32
#心房#
37
房颤,临床上碰到很多哦
48