J Immunother Cancer:转移性Merkel细胞癌采用Avelumab作一线治疗的缓解率
2021-08-04 Nebula MedSci原创
mMCC患者使用Avelumab作为一线治疗可获得40%的缓解率和30%的持久缓解率
Merkel细胞癌(MCC),又名皮肤神经内分泌癌、原发性皮肤类癌、原发性皮肤小细胞癌、原发性神经母细胞瘤等,是一种皮肤侵袭性神经内分泌肿瘤。Merkel细胞癌是目前已知恶性程度最高的原发性皮肤肿瘤,其死亡率为恶性黑色素瘤的2倍,易复发、转移,预后极差。
Avelumab是一种抗DP-L1抗体,已在多个国家获批用于治疗转移性Merker细胞癌(mMCC)。
本文报告了在一项II期临床试验中使用Avelumab作为一线治疗在mMCC患者队列中的疗效和安全性数据,以及探索性的生物标志物分析
该试验受试者为初治的mMCC患者,每两周接受一次Avelumab(10 mg/kg,静滴)治疗。主要终点是缓解持续时间。次要终点包括无进展生存期(PFS)、总生存期(OS)、安全性和生物标志物分析。
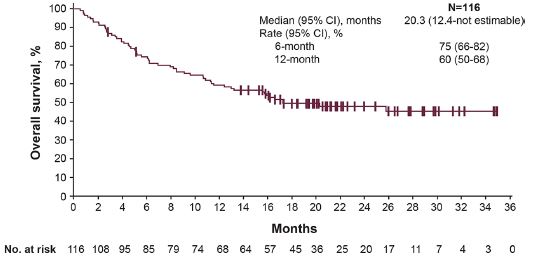
总生存期
共有116位患者接受了Avelumab治疗,中位随访时间为21.2个月。35位患者的缓解持续时间≥6个月,持续缓解率为30.2%。客观缓解率为39.7%。中位PFS为4.1个月,中位OS为20.3个月。
PD-L1+肿瘤、Merkel细胞多瘤病毒 (MCPyV) 阴性肿瘤和瘤内CD8+T细胞密度增加的肿瘤患者的缓解率均高于总体缓解率。探索性分析未发现能够可靠地预测对受试患者对Avelumab一线治疗的反应的生物标志物;但是,一种新的基因表达特征可鉴定MCPyV+肿瘤的存在。
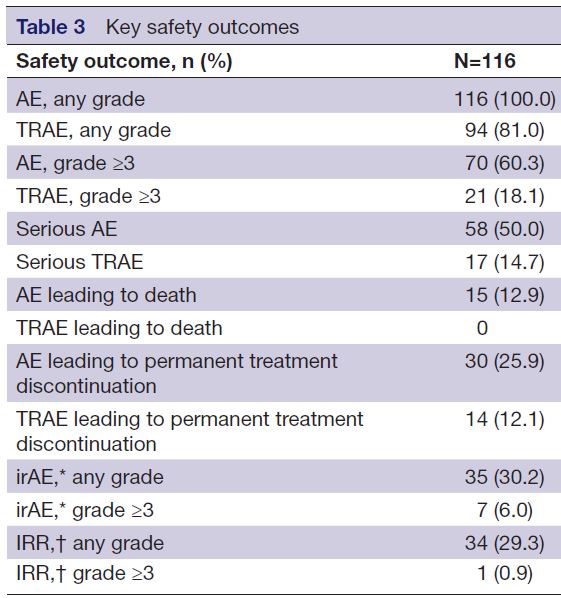
治疗相关不良事件
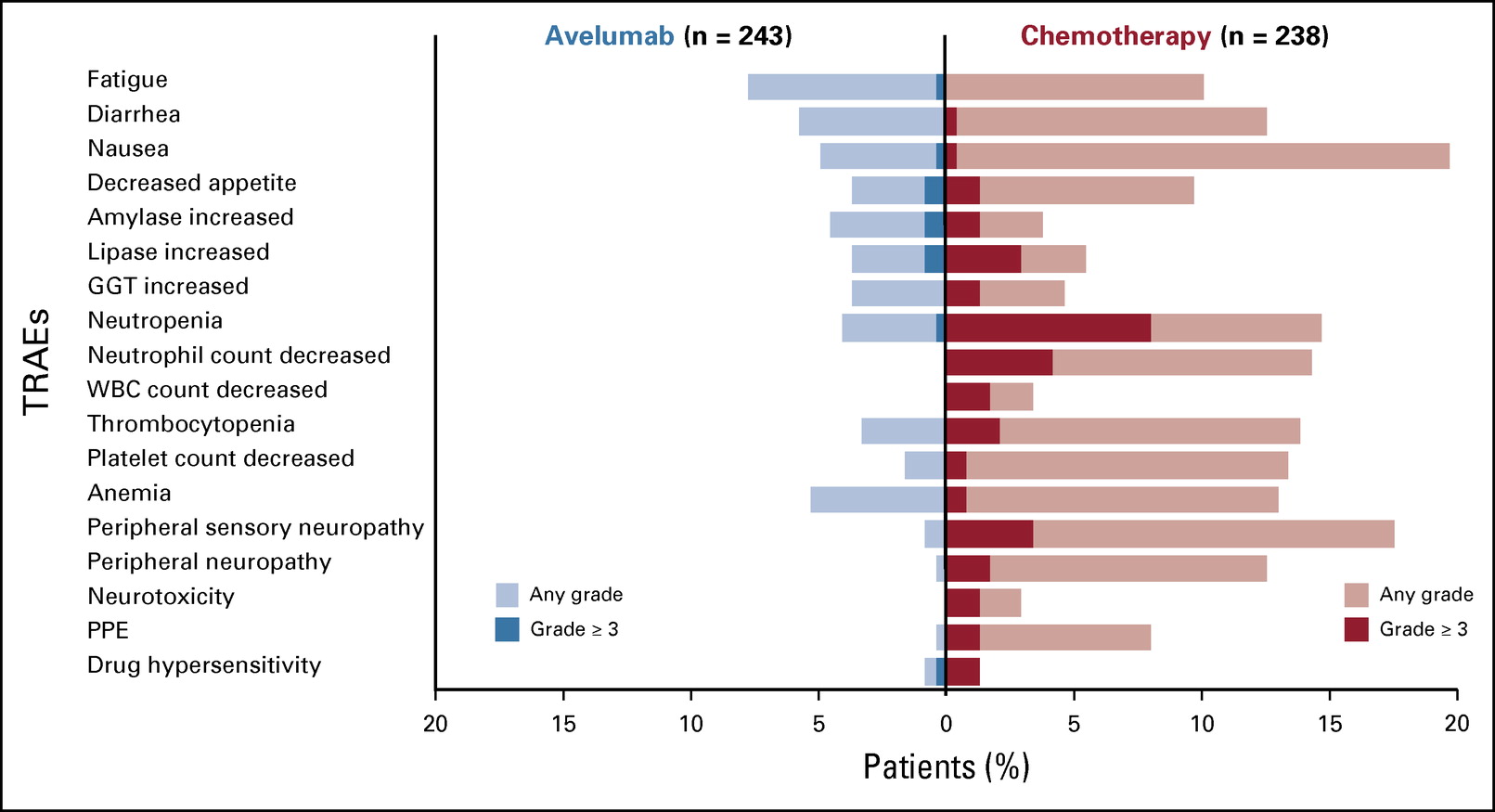
研究期间,共发生了94例 (81.0%) 任何级别的与治疗相关的不良事件,其中3/4级事件21例 (18.1%);无治疗相关死亡发生。
总而言之,mMCC患者使用Avelumab作为一线治疗可获得40%的缓解率和30%的持久缓解率;而且,3/4级治疗相关不良事件的发生率较低。
原始出处:
D'Angelo Sandra P,Lebbé Celeste,Mortier Laurent et al. First-line avelumab in a cohort of 116 patients with metastatic Merkel cell carcinoma (JAVELIN Merkel 200): primary and biomarker analyses of a phase II study.[J] .J Immunother Cancer, 2021, https://doi.org/10.1136/jitc-2021-002646
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#mAb#
23
#细胞癌#
24
#ERK#
26
#avelumab#
32
#转移性#
35
关注医学
60