你是不是也经常在颈动脉超声报告中看到颈动脉斑块字眼?
你是不是经常被患者问颈动脉斑块到底要不要治疗?
你是不是在临床上也发现得颈动脉斑块的人很多?
是的,颈动脉斑块的患病率远超我们的想象!
2017年一项发表在中国循环杂志的中国慢病前瞻性研究分析显示[1],中国有1/3成人存在颈动脉粥样硬化斑块。在40~49岁的年龄段中,仅有6%有斑块,但在70~89岁年龄段中,有63%存在颈动脉斑块。
2020年Lancet子刊上发表的一项调查数据显示[2],我国有近2亿人患有颈动脉斑块。而该课题组之前发表的数据显示,2010年30~79岁国人中,有1.5亿人患有颈动脉斑块。显然,10年间患病人数激增!
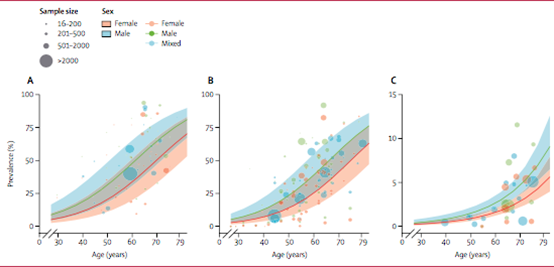 30~79岁人群颈动脉内中膜厚度 (A)、颈动脉斑块 (B) 和颈动脉狭窄 (C)患病率增加(Lancet子刊)
30~79岁人群颈动脉内中膜厚度 (A)、颈动脉斑块 (B) 和颈动脉狭窄 (C)患病率增加(Lancet子刊)
那么,为什么颈动脉容易形成斑块?颈动脉斑块到底是从哪里来的?它有哪些危害?如何治疗和预防?
颈动脉斑块如何形成?
绝大部分的颈动脉斑块是由动脉粥样硬化引起。我们知道,动脉硬化是一个慢性发展的过程,有以下4个阶段:
1、早期阶段:动脉出现脂质条纹;
2、脂质条纹进一步发展为纤维斑块;
3、粥样硬化形成期,动脉内出现灰黄色的斑块;
4、继发病变,包括斑块内出血,斑块破裂,血栓形成,钙化和动脉瘤形成。
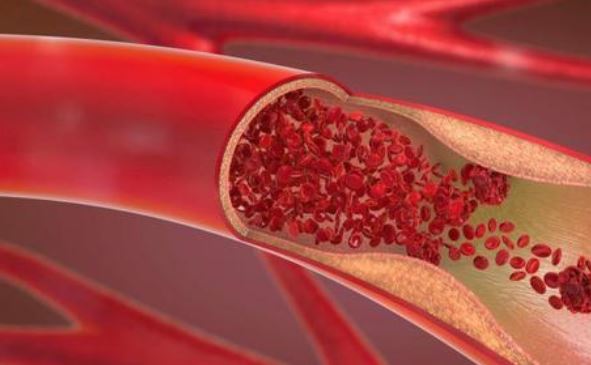
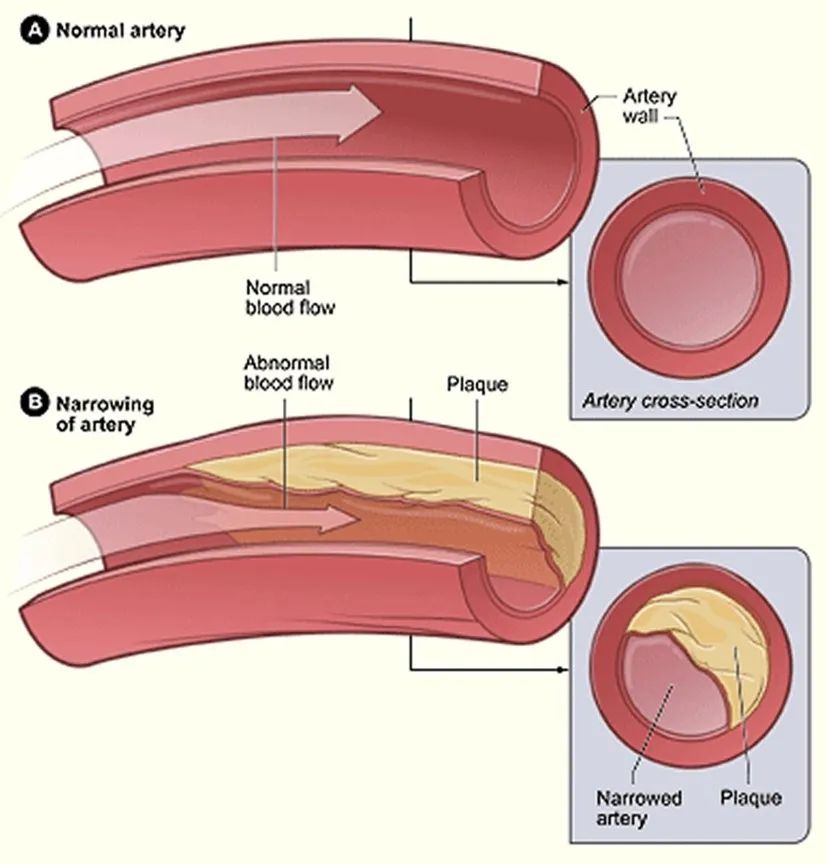 正常的血管与有动脉斑块的血管
正常的血管与有动脉斑块的血管
为什么颈动脉那么容易出现斑块?
这和颈动脉的解剖结构有很大的关系。颈动脉的解剖结构上有一处“Y”型的分支,在此分支处血流冲刷力量大,很容易造成动脉内膜的机械损伤,导致胆固醇从损伤处进入血管内膜,形成斑块。其次,因为颈动脉是距离体表较浅的大型动脉,易于进行超声检查。如果出现了斑块,很容易被发现。
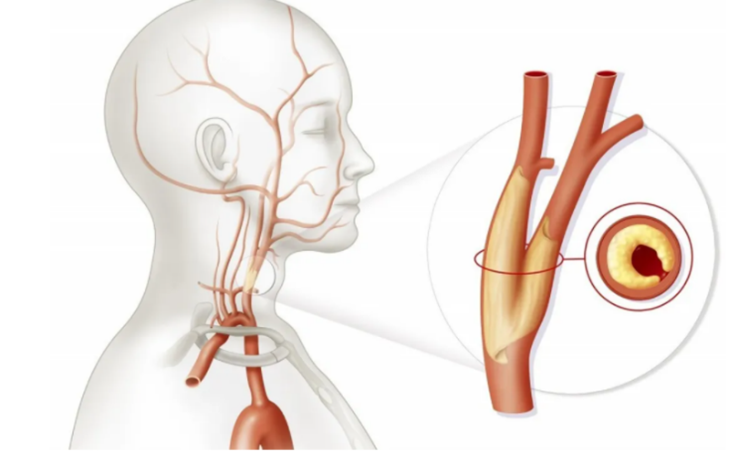 颈动脉解剖图
颈动脉解剖图
颈动脉斑块的危险因素?
尽管有特殊的解剖结构导致颈动脉斑块容易形成,但它并不会无缘无故形成。
颈动脉斑块的形成通常分为可调控和不可调控因素。不可调控因素如年龄、性别和遗传因素等,这是无法改变的。但也有我们可以调控的因素。
2019年一项荟萃分析探讨了颈动脉斑块的可调控危险因素[3],研究人员纳入了1962年~2018年的76项相关性研究,共涉及48847名参与者,结果显示9种危险因素与颈动脉斑块的存在有显著相关性:
高脂血症、高同型半胱血症、高血压、高尿酸血症、吸烟、代谢综合征、高甘油三酯血症、糖尿病、高低密度脂蛋白血症。
其中4种危险因素(高脂血症、高同型半胱氨酸血症、高血压和高尿酸血症)可使颈动脉斑块的风险提高至少30%。
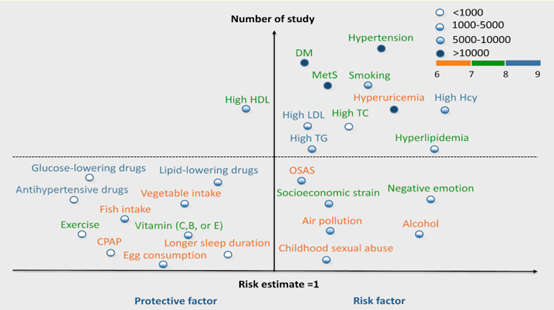 颈动脉粥样硬化可调控因素[3]
颈动脉粥样硬化可调控因素[3]
从这些可调控因素可看出,生活方式的干预在颈动脉斑块的防治中有着至关重要的作用。
颈动脉斑块有什么危害?
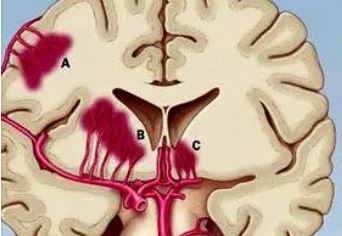
如果颈动脉斑块较小,颈动脉狭窄<50%,患者可能不会出现明显临床症状。但如果颈动脉狭窄超过50%,患者可能出现脑供血不足的相关症状。
除此之外,当斑块不稳定、破裂时,会形成血栓堵塞血管或血栓脱落。若斑块随着血流堵塞脑部,容易引起脑卒中。
《中国脑卒中防治报告(2018)》显示[4],50%~75%的缺血性脑卒中由颈动脉病变所致,严重时可危及生命。
2021年发表在《美国心脏病学会杂志》(JACC)[5]上的一项研究显示,颈动脉粥样硬化斑块中斑块内出血(IPH)的存在是卒中和冠心病的独立危险因素。
该研究纳入2007年~2012年期间,来自基于人群的鹿特丹研究的1349人(平均年龄72岁,49.5%为女性)。参与者此前根据颈动脉超声检查显示亚临床动脉粥样硬化,并对颈动脉进行了高分辨率磁共振成像以评估斑块特征,但并没有卒中或冠心病病史。
研究结果显示,独立于最大斑块厚度和心血管风险因素,IPH的存在与卒中和冠心病的发生有关,分别增加142%与95%的风险(OR=2.42,95CI, 1.30~4.50; OR=1.95,95%CI,1.20~3.14))。
可见,颈动脉斑块和脑卒中、冠心病有着密切的关系。所以,有颈动脉斑块的患者应积极治疗,预防脑卒中和冠心病。
颈动脉斑块要治疗吗?
临床上经常看到患者的彩超报告提示颈动脉斑块,很多人不会引起重视。但事实上,一旦发现颈动脉斑块,就应该积极治疗。
1、积极干预危险因素
-
高血压:颈动脉斑块合并高血压患者应将血压控制<140/90mmHg,如果可以耐受,尽可能控制<130/80 mmHg; -
糖尿病:应控制糖化血红蛋白在7.0%以下; -
高同型半胱氨酸血症:可适量补充叶酸。
-
男性≥50岁或女性绝经期后; -
得到初步控制的高血压(高血压患者经治疗后血压<150/90 mmHg); -
糖尿病; -
高胆固醇血症; -
肥胖(体质量指数≥28); -
早发心血管病家族史(父母一方或双方男性<55岁,女性<65岁发病); -
吸烟。

-
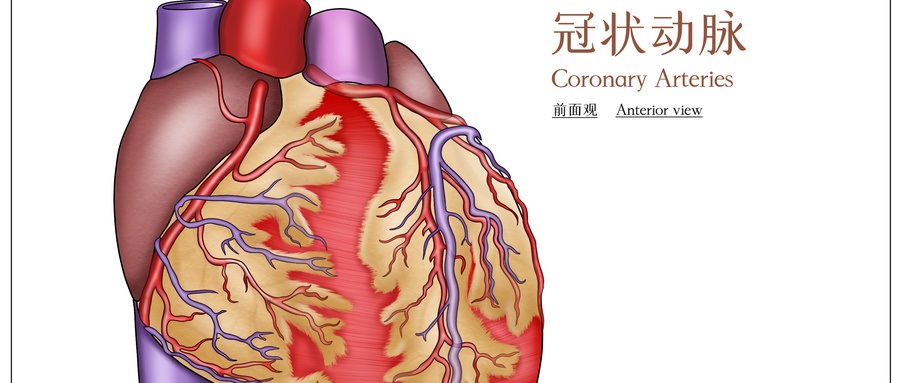
颈动脉内膜切除术(CEA):适应于有症状的颈动脉狭窄,无创检查狭窄≥70%或血管造影狭窄≥50%;或没有症状但血管造影狭窄≥70%。 -
颈动脉支架成形术(CAS):即在颈部血管放支架,利用支架把狭窄的血管管腔给撑起来,与心脏冠状动脉放支架是一个道理。
-
戒烟限酒; -
坚持适量且有规律的运动; -
控制体重; -
改善饮食结构:少吃含饱和脂肪的红肉,多吃鱼和植物蛋白、多吃蔬菜; -
减少压力,避免熬夜; -
定期检测血压、血糖和血脂,一旦发现,积极控制。建议超过50岁男性、绝经后的女性、高血压、糖尿病、高血脂、吸烟、肥胖等人群,最好每年查一次颈动脉超声,能及时发现斑块大小是否稳定。

参考文献:
[1] Clarke R, Du H, Kurmi O, etal. Burden of carotid artery atherosclerosis in Chineseadults: Implications forfuture risk of cardiovascular diseases. Eur J PrevCardiol. 2017Jan1:2047487317689973. doi: 10.1177/2047487317689973.
[2] PeigeSong, PhD,Zhe Fang, MD,Hanyu Wang, BA,et al.Global and regional prevalence,burden, and risk factors for carotid atherosclerosis: a systematic review,meta-analysis, and modelling study.THE LANCET Global Health,2020.
[3] 冀茜.颈动脉粥样硬化可调控危险因素的荟萃分析及系统评价[D].辽宁:大连医科大学,2019.
[4]《中国脑卒中防治报告(2018)》
[5] From Risk Factors toClinical Disease: New Opportunities and Challenges for Cardiovascular RiskPrediction. J Am Coll Cardiol. 2021 Mar, 77 (11)1436–1438.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#颈动脉#
70
#颈动脉斑块#
51
#斑块#
49
内膜损伤
56
三分之一患病,太可怕了
43
不错👍
46