JAMA Netw Open:老年女性每天轻运动5小时,行动障碍发生风险降低40%
2021-02-25 MedSci原创 MedSci原创
迄今为止,几乎所有关于身体活动(PA)的证据,包括2018年PA指南中的证据,都集中在高强度的PA上。有研究显示,中等强度PA计划增加了下肢的身体功能,减少了意外活动的致残率。
预计到2035年,美国65岁以上人口将达到7800万,在美国历史上首次超过18岁以下的儿童。美国人口老龄化的部分原因是预期寿命的增加,所有种族/族裔的女性比男性拥有近5年的长寿优势。然而,在美国,27%的65岁以上人口患有行动障碍,比如行走或爬楼梯的严重困难,也是美国最主要的致残因素。24%的老年女性无法行走2至3个街区,而老年男性的比例为14%。
迄今为止,几乎所有关于身体活动(PA)的证据,包括2018年PA指南中的证据,都集中在高强度的PA上。有研究显示,中等强度PA计划增加了下肢的身体功能,减少了意外活动的致残率。那么,轻度身体活动(LPA),如休闲散步或从事大多数日常生活活动,是否能降低行动障碍的风险,尚不清楚。

近日,发表在JAMA Netw Open杂志的一项研究显示,轻度运动可以保持行动能力,尤其对绝经后女性。在这项前瞻性队列研究中,研究人员收纳了在2012年3月至2014年4月期间参加 "客观测量身体活动和心血管健康研究 “的女性,该研究是 "妇女健康倡议 "的辅助研究,随访至2018年3月31日。"妇女健康倡议 “是一项多站点人群研究,从美国40个临床站点招募。该研究收纳了5735名63岁及以上的女性,平均年龄为78.5岁,其中有2811名白人参与,数据分析时间为2018年8月至2019年5月。

根据分析样本中的分布情况,将LPA的每日平均时数分为四分位数:第一分位数[Q1],LPA的平均时数为0.6至4.0小时/天;第二分位数[Q2],LPA的平均时数4.0至4.8小时/天;第三分位数[Q3],LPA的平均时数4.8至5.6小时/天;第四分位数[Q4],LPA的平均时数5.6至10.4小时/天。
结果显示,与轻强度体力活动第四分位数的女性相比,在第二分位数(多变量危险比[HR],0.78;95% CI,0.67-0.90)、第三分位数(HR,0.60;95% CI,0.51-0.71)和第四分位数(HR,0.60;95% CI,0.51-0.71)中观察到较低的意外行动障碍风险。在第二分位数(多变量HR,0.72;95% CI,0.60-0.85)、第三分位数(HR,0.55;95% CI,0.46-0.67)和第四分位数(HR,0.52;95% CI,0.42-0.63)中,这种有益的关联对持续性活动障碍更强(P < .001)。进一步分层分析显示,与体重指数为30.0或更高的女性相比,较轻体重指数小于30.0的女性(HR,0.73;95% CI,0.66-0.82)的关联性更强(HR,0.91;95% CI;0.79-1.04)。
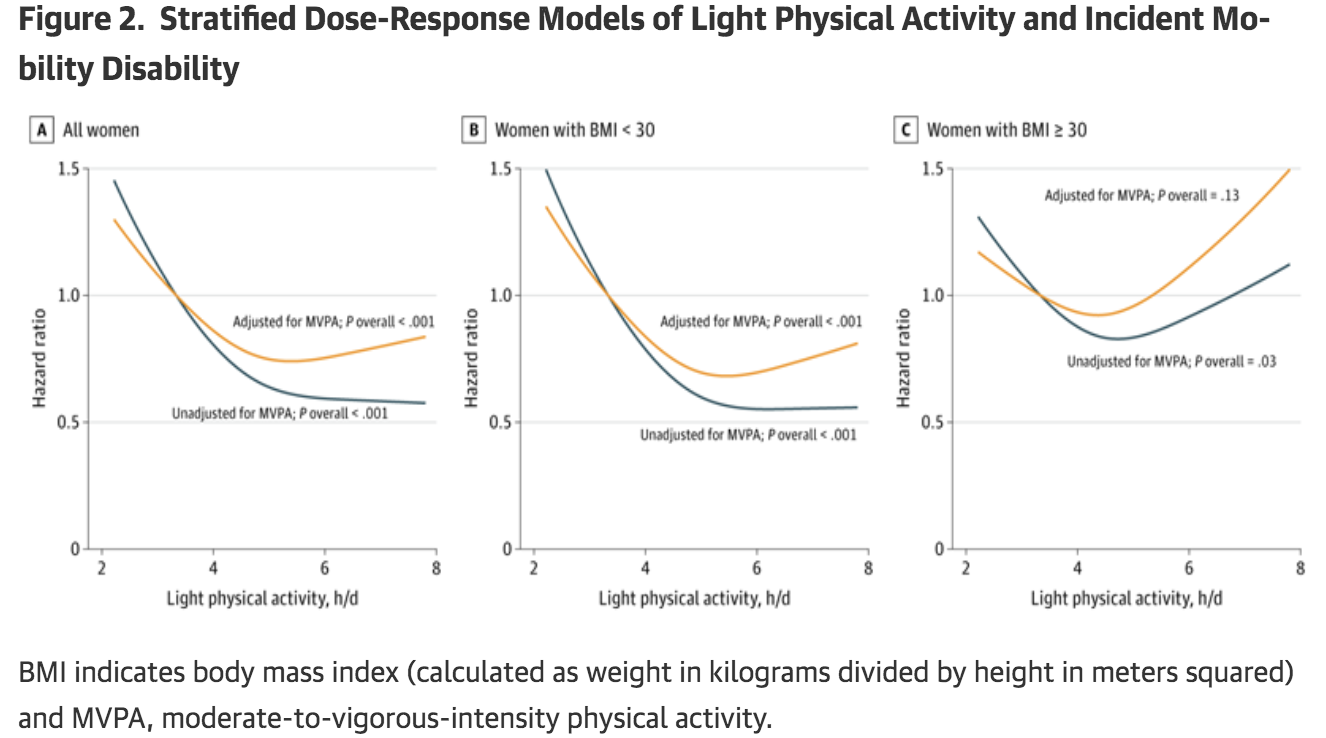
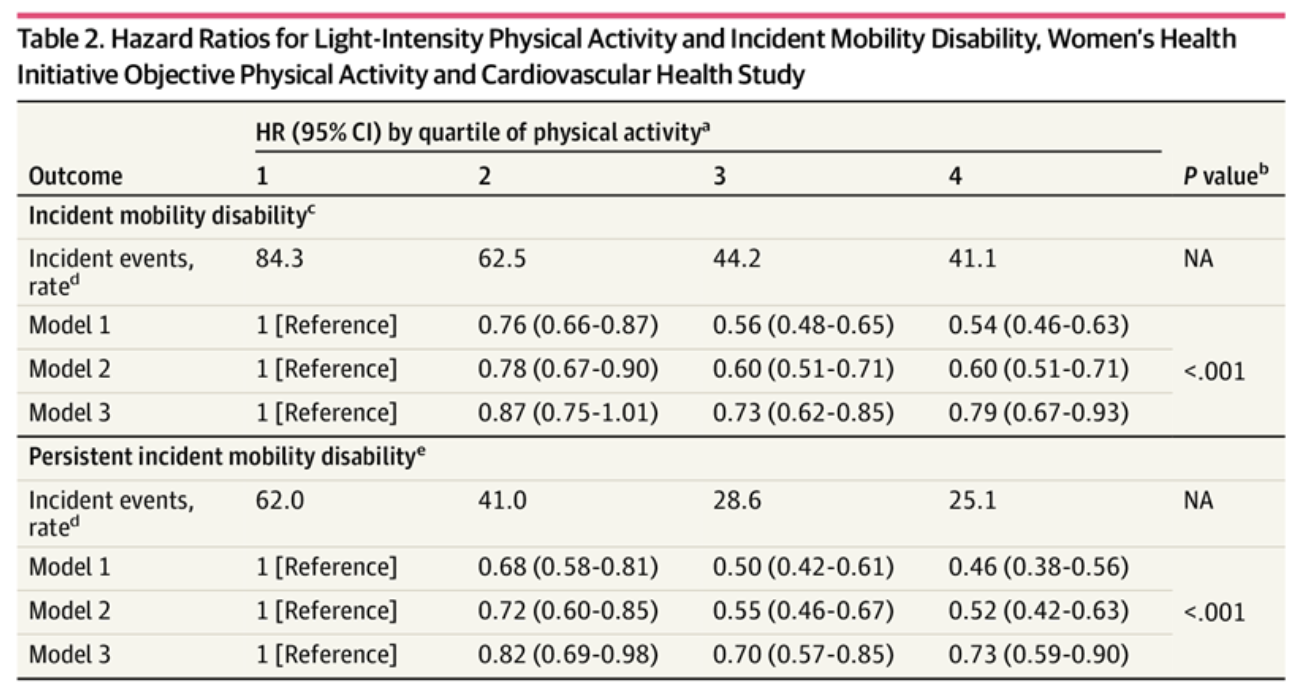
总之,从LPA的第二低分位数开始,随着LPA的增加,发生意外行动障碍的风险降低。与LPA最低四分位数的女性相比,LPA最高四分位数的女性发生行动障碍的风险降低了40%,持续行动障碍的风险降低了48%。因此,高水平的LPA对于降低行动不便的风险是不必要的,因为在每天大约5小时的LPA中没有显著性改变。
原始出处:
Nicole L. Glass, MPH1; John Bellettiere, PhD1; Purva Jain, MPH1; et al.Evaluation of Light Physical Activity Measured by Accelerometry and Mobility Disability During a 6-Year Follow-up in Older Women.JAMA Netw Open. 2021;4(2):e210005. doi:10.1001/jamanetworkopen.2021.0005
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PE#
34
#风险降低#
36
#NET#
33
学习
71
学习
58
学习了!!!
87
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
47