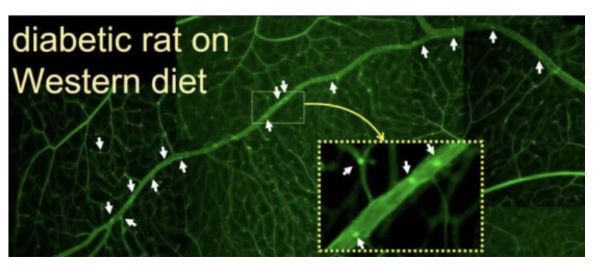
JAMA Otolaryngol Head Neck Surg:视网膜微血管征和年龄相关的听力损失相关性研究
2020-01-16 AlexYang MedSci原创
年龄相关的听力损失是高度可预防和治疗的,理解该疾病的病因对疾病的预防可能有帮助。最近,有研究人员调查了是否微血管征与年龄相关的听力损失相关。研究包括了1458名个体(平均年龄(SD),76.1(5.0)岁(年龄范围67-90岁);825名女性(56.6%);285名黑人(19.5%))。在具有或者不具有视网膜疾病的个体中,每dB听力水平PTA的差异为2.21(95%CI, -0.22到4.63),
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#年龄相关#
35
#NEC#
31
#相关性#
42
#视网膜#
38
#听力#
34
#微血管#
32
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
52