Ann Surg:食管裂孔疝对食管或交界处腺癌术后的预后影响
2016-11-01 MedSci MedSci原创
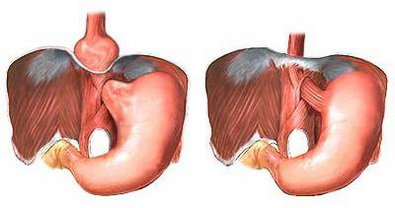
评估食管裂孔疝(HH)≥5 厘米(HH组) vs 没有HH或HH<5 厘米(对照组)患者的肿瘤完整切除率(主要目的)、术后30天结局和生存(次要目标)。HH是食管或交界处腺癌(EGJA)的危险因素。EGJA术后HH对结局的影响仍是未知的。367例接受手术治疗的EGJA患者,通过CT和钡餐寻找HH,比较HH (n = 42)组和对照组(n = 325)。在HH组,EGJAs的不完全切除率更高(50.
评估食管裂孔疝(HH)≥5 厘米(HH组) vs 没有HH或HH<5 厘米(对照组)患者的肿瘤完整切除率(主要目的)、术后30天结局和生存(次要目标)。
HH是食管或交界处腺癌(EGJA)的危险因素。EGJA术后HH对结局的影响仍是未知的。
367例接受手术治疗的EGJA患者,通过CT和钡餐寻找HH,比较HH (n = 42)组和对照组(n = 325)。
在HH组,EGJAs的不完全切除率更高(50.0% vs 4.0%; P < 0.001),pN3期更多(28.5% vs 10.1%; P = 0.002),中位生存更低(20.9 vs 41.0个月; P = 0.001)。调整后,HH≥5 厘米是不完全切除(OR 21.0, 95% CI 9.4-46.8, P < 0.001)和不良预后(HR 1.6, 95% CI 1.1-2.5, P = 0.025)的预测因素。在HH组,接受新辅助放疗的患者,其30天死亡率明显更高(20.0% vs 0%; P = 0.040),这与更大的心脏和肺毒性有关。
这是第一次,我们发现,HH≥5 厘米与EGJA术后更差的预后有关,与更大的不完全切除率和更多的淋巴结受累有关,新辅助放疗对这类患者具有明显的毒性。
原始出处:
Gandon A1, Gronnier C,et al.Esophageal Adenocarcinoma: Impact of a Large Hiatal Hernia on Outcomes After Surgery.Ann Surg. 2016 Nov;264(5):862-870.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#食管裂孔疝#
37
#食管#
26
#疝#
26
好好好学习了分享
50
这个可以的~
49