IBD:血清5-羟色胺可以区分克罗恩病患者的疾病活动度
2020-08-26 MedSci原创 MedSci原创
炎症性肠病(IBDs)是胃肠道系统的慢性炎症性疾病,可分为2种主要的亚型:溃疡性结肠炎(UC)和克罗恩氏病(CD)。
炎症性肠病(IBDs)是胃肠道系统的慢性炎症性疾病,可分为2种主要的亚型:溃疡性结肠炎(UC)和克罗恩氏病(CD)。 IBD的诊断和预后评估主要依靠昂贵且耗时的内窥镜检查,组织学检查和射线照相检查,非侵入性检查较少见。目前有大量证据表明神经激素5-羟色胺(5-羟色胺,5-HT)参与了IBD的病理生理,在胃肠道中,5-HT可以增强肠道运动能力,参与神经元反射,并调节液体和电解质的运输。因此,本项研究旨在探究活动性溃疡性结肠炎(UC)或克罗恩病(CD)患者血清5-HT是否升高。
研究人员收集了在2005年至2010年从德国雷根斯堡大学医学中心内科中确诊为UC或CD的患者的血清样品。根据临床疾病评估,研究人员将患者分为活动性疾病,难治性疾病或处于缓解状态的疾病。对于CD,克罗恩病活动指数(CDAI)<150表示缓解,而CDAI> 150则表示活动性疾病。同时研究人员使用高压液相色谱法测量血清样品中的5-HT水平,色氨酸(TRP)和犬尿氨酸(KYN)水平,并使用ELISA测量细胞因子水平。
该研究共纳入96名经确诊IBD诊断的患者,其中45名CD患者,46名UC患者。在45例CD患者中,有15例处于缓解状态,15例患 有活动性疾病,15例患有难治性疾病。在45例UC患者中,有15例处于缓解状态,15例患有活动性疾病,16例患有难治性疾病。
研究人员首先测量了UC和CD患者的血清中TRP,5-HT和KYN的水平,并在疾病类别之间进行了比较。在UC中,所测代谢物在缓解期患者,活动性疾病患者或难治性疾病患者之间均无区别,但在CD中,疾病类别之间的TRP或KYN水平没有统计学上的显着差异,但是活动性疾病患者的5-HT显着增加。同时,与活动性疾病(P=0.13)或难治性疾病(P=0.060)的患者相比,缓解期患者的CRP呈下降趋势。但是,CRP水平无法区分CD中的疾病状态,在区分CD中的疾病类别方面,血清5-HT优于C反应蛋白和循环细胞因子。
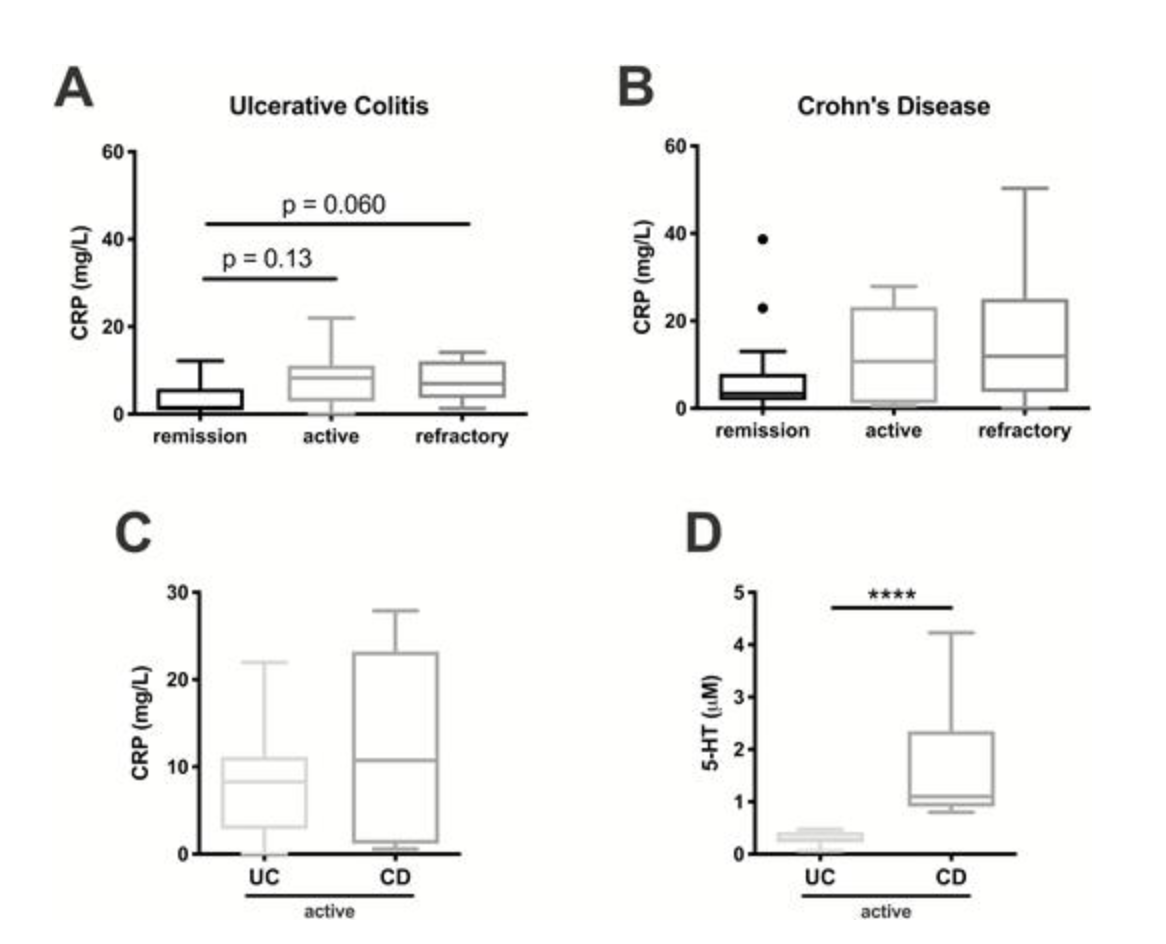
因此,研究人员说道:血清5-HT可以区分CD患者之间的活动性疾病和难治性疾病或缓解,血清5-HT是一种作为诊断活动性CD的有效生物标志物。
原始出处:
Christopher R Manzella. Et al. Serum Serotonin Differentiates Between Disease Activity States in Crohn’s Patients. Inflammatory Bowel Diseases.2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#活动度#
40
#疾病活动#
36
#疾病活动度#
27
学习
80
#IBD#
29
学习了,谢谢分享
86
学习了
72
相关资讯请继续分享,谢谢
83
很好很详细,谢谢分享
80
学习了
29