Plos Med:葡萄糖凝胶有效降低新生儿低血糖发生率,但无法减少重症监护病房入院率
2021-02-23 MedSci原创 MedSci原创
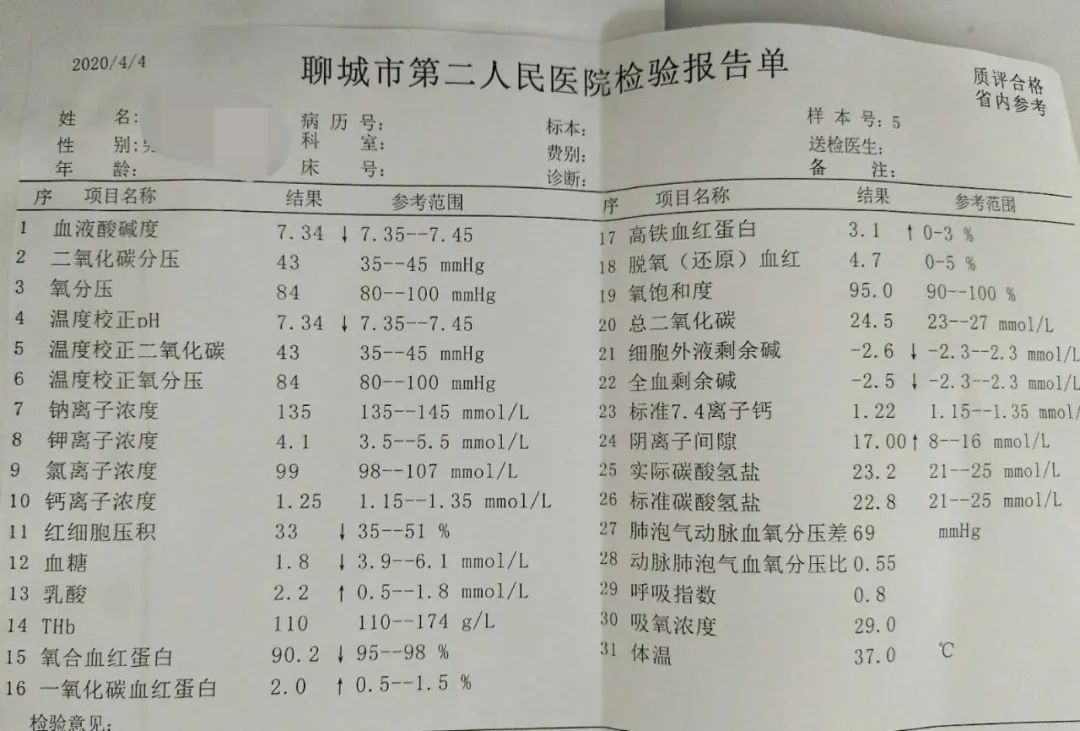
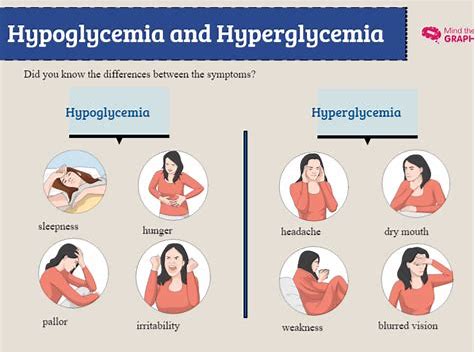
低血糖症是指由多种原因引起的血糖浓度过低所致的综合征。一般以血浆血糖浓度<2.8mmol/L,或全血葡萄糖<2.5mmol/L为低血糖。儿童低血糖诊断标准比成人值低1.11mmol/L。低
低血糖症是指由多种原因引起的血糖浓度过低所致的综合征。一般以血浆血糖浓度<2.8mmol/L,或全血葡萄糖<2.5mmol/L为低血糖。儿童低血糖诊断标准比成人值低1.11mmol/L。低血糖症在新生儿中很常见,多项研究显示,即使是暂时性的,也可导致脑损伤。
目前,葡萄糖凝胶被广泛用于治疗新生儿低血糖症,便宜且安全。先前的一项研究表明,单剂量200mg/kg预防性葡萄糖凝胶可以降低高危婴儿低血糖的发生。但尚不清楚这是否可以改善临床上重要的结局,例如新生儿重症监护。近日,发表在Plos Med杂志的一项研究显示,200mg/kg预防性葡萄糖凝胶并不能降低新生儿重症监护室(NICU)的入院率,但可以降低低血糖症。
在这项随机对照试验中,研究人员对来自2015年1月至2019年5月新西兰和澳大利亚的18家妇产医院2149名婴儿,并将其随机分配至葡萄糖凝胶组和安慰剂组。主要结局为重症监护病房(NICU)入院以及住院时间超过4小时。次要结局包括低血糖,因低血糖而入住NICU,高血糖,出院时母乳喂养,6周时配方奶喂养和产妇满意度。
研究结果显示,98%的新生儿接受了葡萄糖凝胶治疗,并且耐受性良好。新生儿NICU的总体入院率为9.9%,与葡萄糖凝胶组和安慰剂组因低血糖而发生NICU入院相似,分别为10.4%和9.4%。
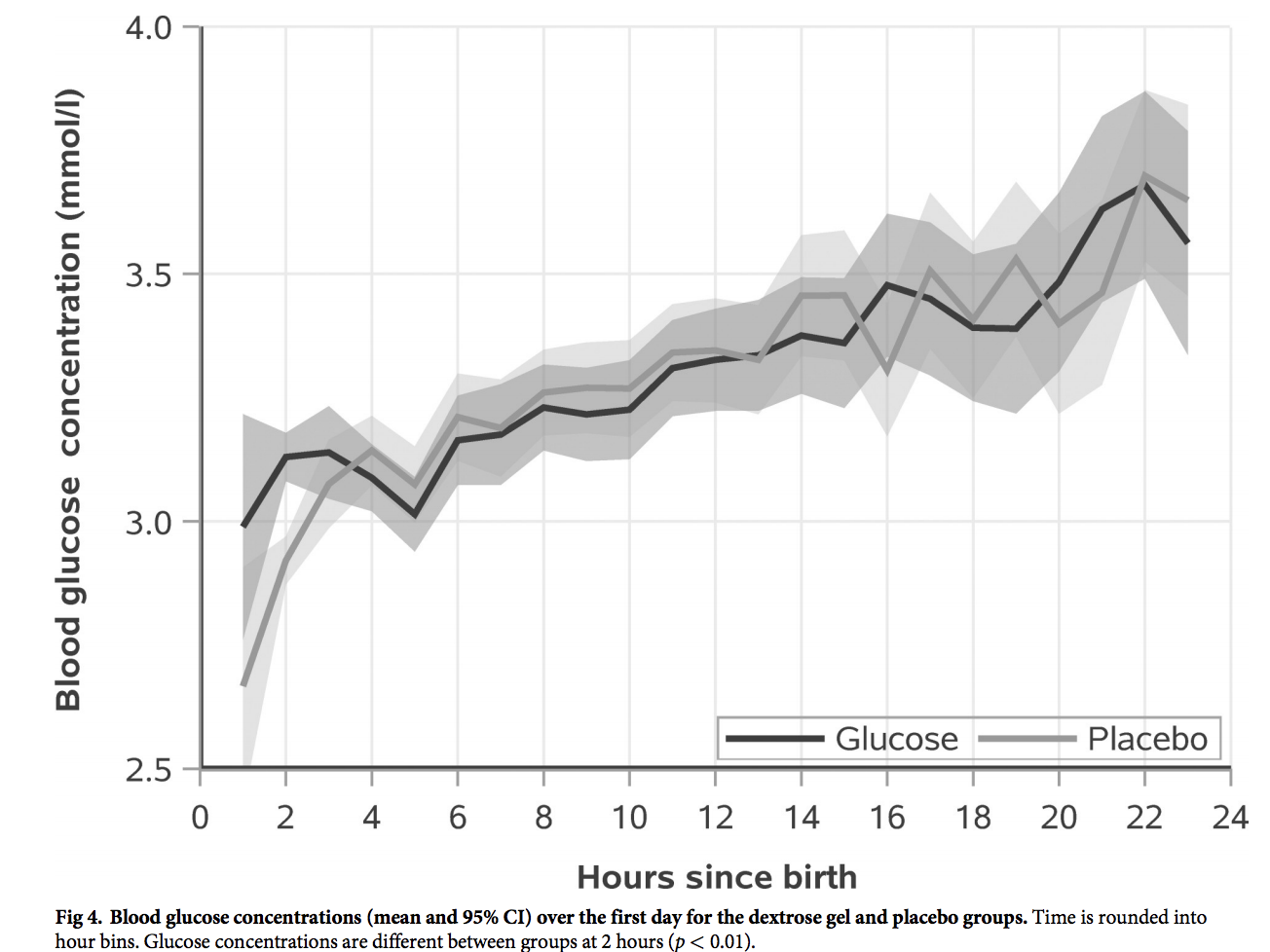
然而,在葡萄糖凝胶组,新生儿几乎没有发生低血糖事件。在出院时母乳喂养(aRR 1.00;95% CI 0.99,1.02;p = 0.67)、出院前接受配方奶(aRR 0.99;95% CI 0.92,1.08;p = 0.90)、6周时配方奶喂养(aRR 1.01;95% CI 0.93,1.10;p = 0.81)等方面组间无差异,且无高血糖发生。
总之,预防性葡萄糖凝胶并没有减少NICU入院人数,然而,它确实减少了低血糖的发生率。因此,临床医生和临床指南组应考虑将其预防性葡萄糖凝胶引入临床实践,进而更好的筛查新生儿低血糖发生的发病率,以预防脑损伤。未来,需要对更大规模数据进行随访,进一步评估预防性葡萄糖凝胶在预防新生儿低血糖症中的临床效用。
原始出处
Jane E. Harding et al.Evaluation of oral dextrose gel for prevention of neonatal hypoglycemia (hPOD): A multicenter, double-blind randomized controlled trial.Plos Med.2021.https://doi.org/10.1371/journal.pmed.1003411
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#发生率#
49
#低血糖发生率#
58
有没有具体的使用标准啊?
86
#新生儿低血糖#
61
#重症监护病房#
57
#凝胶#
40
#监护#
29
#Med#
51
共同进步
93