Neurology:斜坡后硬膜下血肿所致Godtfredsen综合征
2018-09-27 zyx整理 神经科病例撷英拾粹
30岁女性,表现为突发头痛2天。由于心脏机械瓣膜植入,患者每天服用华法林7.5mg(国际标准化比值3.5)。
30岁女性,表现为突发头痛2天。由于心脏机械瓣膜植入,患者每天服用华法林7.5mg(国际标准化比值3.5)。
患者存在孤立性双侧第6和左侧第12颅神经麻痹(图1),第5颅神经不受累。
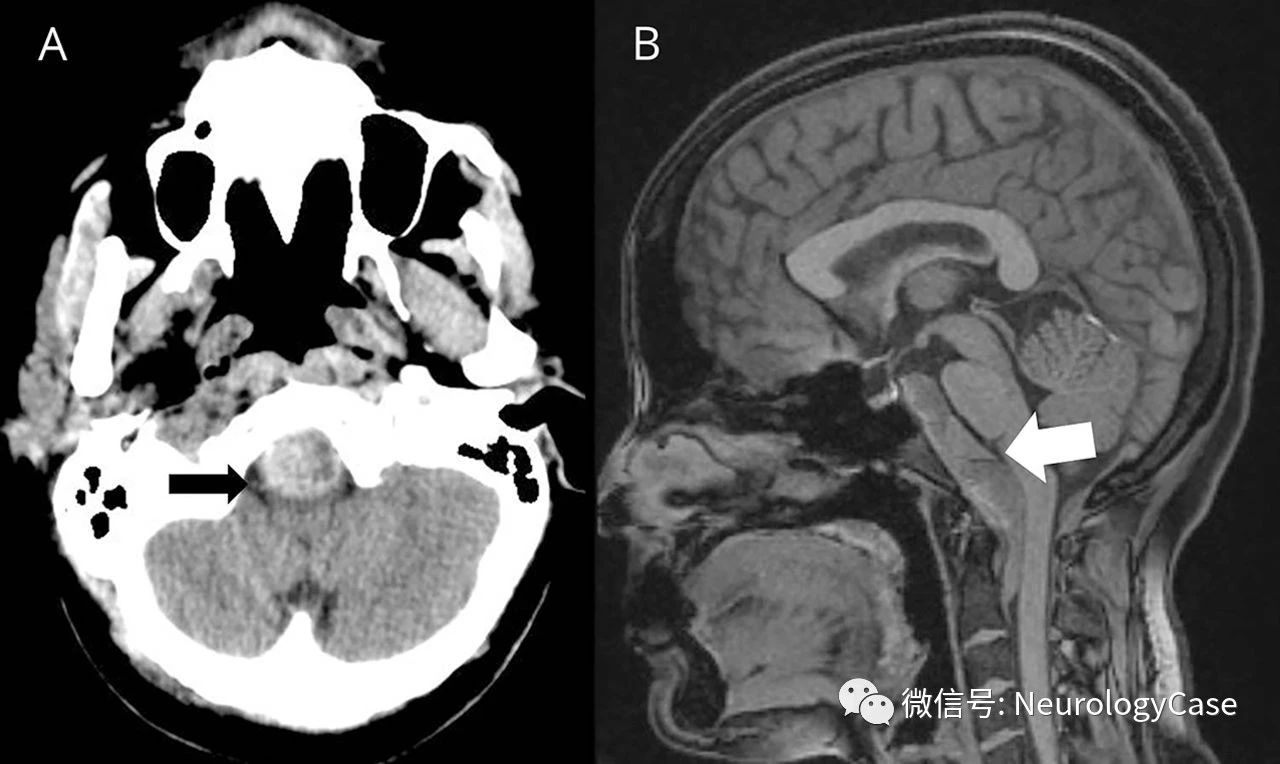
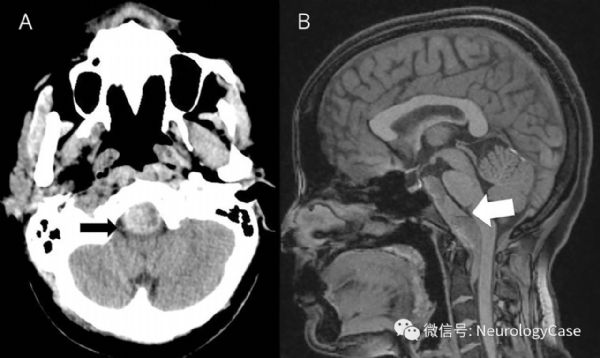
影像学可见斜坡后硬膜下血肿,从后床突延伸至C2椎体,伴脑干受压(图2)。
第6和第12颅神经麻痹的独特组合有助于将病变定位于斜坡(Godtfredsen综合征或clival综合征)。
值得注意的是,Godtfredsen将第6颅神经麻痹归因于鼻咽癌侵犯海绵窦,而第12颅神经麻痹则因咽后淋巴结转移所致。
(图1:患者往左侧注视时,可见左眼外展受损[左侧第6颅神经麻痹],伸舌左偏[左侧第12颅神经麻痹])
(图2:A:头颅CT可见斜坡后血肿[黑箭];B:MRI可见硬膜下血肿[白箭]延伸至C2椎体)
原始出处:Amalnath SD. Teaching NeuroImages: Godtfredsen syndrome due to retroclival subdural hematoma. Neurology. 2018 Sep 4;91(10):e999-e1000.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#硬膜下#
33
#Neurol#
0
#血肿#
27
#硬膜下血肿#
23
#综合征#
32