Eur Heart J:糖尿病合并冠状动脉疾病患者经皮或手术血运重建术后10年全因死亡比较
2021-08-18 MedSci原创 MedSci原创
无论是否伴有糖尿病,PCI与CABG对3VD和/或LMCAD患者10年全因死亡的治疗效果相似。然而,在接受胰岛素治疗的糖尿病患者中,CABG可能有生存获益。
近日,心血管领域权威杂志Eur Heart J上发表了一篇研究文章,该研究旨在比较糖尿病患者或非糖尿病患者在冠状动脉旁路移植术(CABG)或经皮冠状动脉介入术(PCI)后10年的全因死亡率。
 该研究评估了1800名随机接受PCI或CABG治疗的三支血管疾病(3VD)和/或左主干冠状动脉疾病(LMCAD)患者10年期间的生存率。根据糖尿病状态和血运重建策略评估了参与者的10年全因死亡。
该研究评估了1800名随机接受PCI或CABG治疗的三支血管疾病(3VD)和/或左主干冠状动脉疾病(LMCAD)患者10年期间的生存率。根据糖尿病状态和血运重建策略评估了参与者的10年全因死亡。
 在糖尿病患者(n=452)中,5年时,采用PCI治疗的患者的死亡风险在数值上高于采用CABG治疗的患者[19.6% vs. 13.3%,风险比(HR):1.53,95%置信区间(CI):0.96,2.43,P=0.075],而在5到10年之间则相反(PCI vs. CABG:20.8% vs. 24.4%,HR为0.82,95%CI为0.52,1.27,P=0.366)。
在糖尿病患者(n=452)中,5年时,采用PCI治疗的患者的死亡风险在数值上高于采用CABG治疗的患者[19.6% vs. 13.3%,风险比(HR):1.53,95%置信区间(CI):0.96,2.43,P=0.075],而在5到10年之间则相反(PCI vs. CABG:20.8% vs. 24.4%,HR为0.82,95%CI为0.52,1.27,P=0.366)。
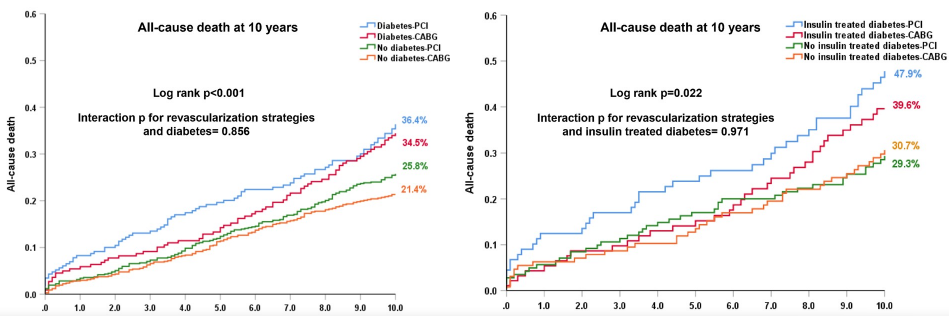 不考虑糖尿病状态,接受PCI或CABG治疗的患者10年时的全因死亡无显著差异,糖尿病患者的绝对治疗差异为1.9%(PCI vs. CABG:36.4% vs. 34.5%,差异:1.9%,95%CI:-7.6%,11.1%,P=0.551)。在接受胰岛素治疗的糖尿病患者中(n=182),接受PCI治疗的患者10年的全因死亡率相比于CABG治疗的患者更高(47.9% vs. 39.6%,差异:8.2%,95%CI为-6.5%,22.5%,P=0.227)。
不考虑糖尿病状态,接受PCI或CABG治疗的患者10年时的全因死亡无显著差异,糖尿病患者的绝对治疗差异为1.9%(PCI vs. CABG:36.4% vs. 34.5%,差异:1.9%,95%CI:-7.6%,11.1%,P=0.551)。在接受胰岛素治疗的糖尿病患者中(n=182),接受PCI治疗的患者10年的全因死亡率相比于CABG治疗的患者更高(47.9% vs. 39.6%,差异:8.2%,95%CI为-6.5%,22.5%,P=0.227)。
由此可见,无论是否伴有糖尿病,PCI与CABG对3VD和/或LMCAD患者10年全因死亡的治疗效果相似。然而,在接受胰岛素治疗的糖尿病患者中,CABG可能有生存获益。血运重建策略与糖尿病患者的长期缺血和安全结局之间的关联需要在进一步研究。
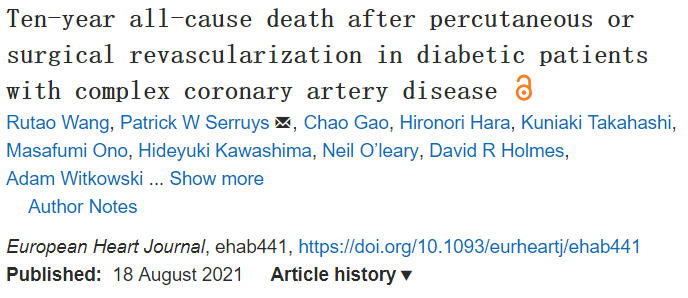
原始出处:
Rutao Wang.et al.Ten-year all-cause death after percutaneous or surgical revascularization in diabetic patients with complex coronary artery disease.European Heart Journal.2021.https://doi.org/10.1093/eurheartj/ehab441
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#血运重建术#
58
#疾病患者#
58
很明确
83
#冠状动脉疾病#
52
#ART#
39
#HEART#
47
学习了
82
学习学习
100
谢谢MedSci提供最新的资讯
69
学习
102