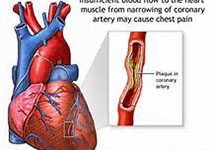
Eur Heart J:缺血性心脏T细胞反应的表型研究
2019-12-31 不详 MedSci原创
心肌梗死引起的持续性心脏T细胞反应与随后的不良心室重塑和心力衰竭进展有关,目前尚无T细胞受体(TCR)剧集的变化与缺血心力衰竭心脏T细胞表型特征结合的数据。通过高通量测序对TCR基因序列的分析发现,与对照心脏的T细胞相比,缺血衰竭心脏的TCR基因序列呈克隆性扩展,但TRBV-J重排和V基因片段的使用模式相似。与外周血T细胞相比,缺血衰竭心脏中的T细胞具有限制性和克隆性扩张的TCR序列,TRBV-J
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#缺血性#
29
#T细胞反应#
33
#ART#
27
#表型#
21
#HEART#
34