Eur J Cancer:Rucaparib治疗BRCA1/2野生型转移性乳腺癌的疗效
2021-11-29 Nebula MedSci原创
小部分不携带胚系BRCA1/2突变的高LOH评分患者也可从PARP抑制剂中获益
乳腺癌常携带导致同源重组缺陷(HRD)的基因组变异。已有三项3期临床试验证实,PARP抑制剂可有效治疗携带胚系(g)BRCA1/2突变的HER2阴性(HER2-)转移性乳腺癌。
本研究是一项单臂的2期RUBY试验,旨在评估PARP抑制剂Rucaparib在具有高基因组杂合性丢失 (LOH) 评分或非胚系 BRCA1/2 突变的 HER2-转移性乳腺癌中的疗效。
共有40位符合条件的患者至少服用了一剂Rucaparib被纳入分析。主要终点是临床获益率(CBR)。该研究试验两阶段Simon设计,CBR界值被定为20%。
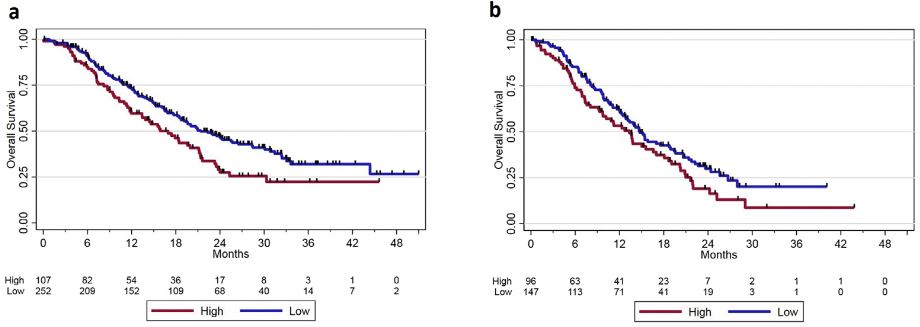
高LOH评分 vs 低LOH评分患者的总生存率:a. ER+/HER2阴性乳腺癌;b. 三阴性乳腺癌
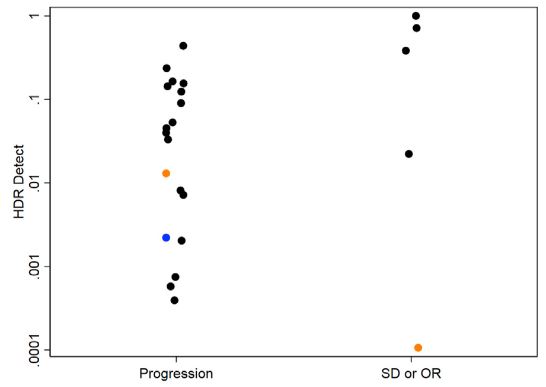
主要终点未达到,临床获益率仅有13.5%。两位高LOH评分、BRCA1/2野生型的患者表现出完全且持久的缓解(分别持续缓解了12个月和28.5个月)。对24例样本(包括5位从Rucaparib治疗中获益的患者)进行了全基因组分析。HRDetect 倾向与患者对Rucaparib治疗的反应相关,但无统计学差异(中位HRDetect应答者 vs 无应答者:0.465 vs 0.040;p=0.2135)。最后,在RUBY试验上游筛查LOH的711位转移性乳腺癌患者中有220位为高LOH评分,分析显示,高LOH评分与更高的死亡可能性相关。
HRDetect评分与肿瘤对Rucaparib反应的相关性
总之,该研究结果提示,小部分不携带胚系BRCA1/2突变的高LOH评分患者也可从PARP抑制剂中获益。但是,该研究结果强调需要开发额外的生物标志物来选择性地识别潜在的可从RARP抑制剂治疗中获益的BRCA1/2野生型乳腺癌患者。
原始出处:
Patsouris Anne,Diop Kadija,Tredan Olivier et al. Rucaparib in patients presenting a metastatic breast cancer with homologous recombination deficiency, without germline BRCA1/2 mutation.[J] .Eur J Cancer, 2021, 159: 283-295.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#CAP#
65
#野生型#
42
#APA#
49
#转移性#
39
#BRCA1#
61
#BRCA1/2#
61
#BRCA#
34
前列腺癌的前列腺特异性抗原 (PSA) 筛查导致
58
好
66