Diabetologia:2型糖尿病患者长期使用二甲双胍与肺炎和相关死亡的风险相关
2021-09-11 从医路漫漫 MedSci原创
二甲双胍对2型糖尿病患者严重呼吸道感染风险增加的长期影响尚不清楚。

目的:二甲双胍对2型糖尿病患者严重呼吸道感染风险增加的长期影响尚不清楚。本研究旨在评估二甲双胍对中国2型糖尿病患者队列中首次因肺炎住院和肺炎相关死亡风险的影响。
方法:研究人员对2001年至2018年在香港糖尿病登记处登记的22,638名2型糖尿病患者进行了回顾性分析,随访至2019年12月31日。采用重叠倾向评分加权来平衡基线特征。在22,638例2型糖尿病患者中,排除了未使用任何降糖药物 (GLDs)和/或eGFR≤30ml min - 1[1.73 m] - 2或基线时接受透析和/或胰岛素治疗的患者,在平均7.5年的随访期间,我们纳入了15,784名长期或偶然使用二甲双胍和917名使用其他GLDs者。
结果:重叠加权分析显示,与使用其他GLDs者相比,二甲双胍患者首次肺炎住院的危险度为0.63 (95% CI 0.52, 0.77),肺炎相关死亡的危险度为0.49 (95% CI 0.33, 0.73);进行性别和肾功能分层后有着类似的观察结果。通过分析显示,二甲双胍暴露时间(总随访时间中二甲双胍处方持续使用时间的比例)与肺炎事件之间也存在负相关。与未使用二甲双胍者相比,二甲双胍使用者首次肺炎住院时中性粒细胞/淋巴细胞比率较低(平均[95% CI]: 12.8 [12.1, 13.5] vs 14.8 [12.3, 17.3],p= 0.032)。二甲双胍相关乳酸酸中毒的发生率为2.5/10万人/年。与其他GLDs使用者相比,二甲双胍使用者发生肺炎事件的风险更低。
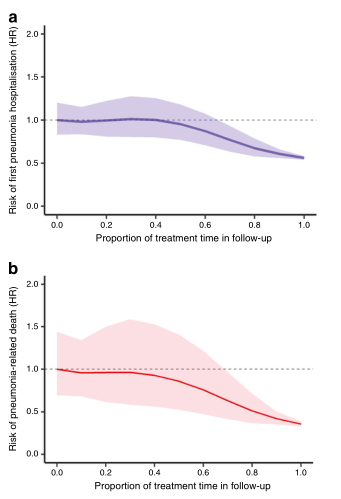
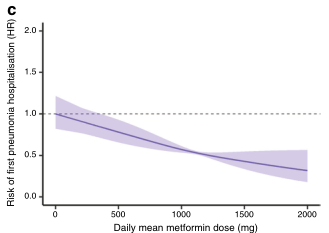
图 曲线显示二甲双胍观察期间肺炎住院(a)和相关的肺炎死亡(b)以及重叠加权队列中二甲双胍每日平均剂量与首次肺炎住院风险之间的关系(c)。阴影部分代表95%的CIs。
肺炎相关死亡定义为首次肺炎住院治疗后≤30天因任何原因死亡。(c)显示使用二甲双胍的Cox回归模型的结果,校正了时变的HbA1c、血脂、年龄、药物和并发症
结论:在中国糖尿病患者中,长期使用二甲双胍与降低肺炎风险和肺炎相关死亡相关。这些结果与其他呼吸道感染的相关性还需进一步研究。
原文出处
Aimin Yang,Mai Shi,Hongjiang,et al,WuLong-term metformin use and risk of pneumonia and related death in type 2 diabetes: a registry-based cohort study.Diabetologia 2021 Aug;64(8)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#DIA#
32
#长期使用#
40
#BET#
46
#2型糖尿病患者#
34
#糖尿病患者#
47
不愧为神药
81
二甲双胍,神药!
71
谢谢MedSci提供最新的资讯
69
谢谢MedSci提供最新的资讯
76