J Thromb Haemost:他汀类药物用于减少静脉血栓栓塞患者静脉事件
2021-10-01 MedSci原创 MedSci原创
该预试验的结果支持开展更大规模随机对照试验,以明确辅助瑞舒伐他汀对VTE二级预防的疗效。
他汀类药物可能会降低复发性静脉血栓栓塞(VTE)的风险,但是,没有随机试验对这一假设进行验证。

近日,血栓和凝血疾病权威杂志Journal of Thrombosis and Haemostasis上发表了一篇研究文章,研究人员进行了一项随机预试验,以明确采用瑞舒伐他汀对VTE进行二级预防的可行性。
新诊断的有症状的近端深静脉血栓形成和/或肺栓塞且接受标准抗凝治疗的患者被随机分配至每天一次20mg瑞舒伐他汀辅助治疗,持续180天,或不采用瑞舒伐他汀治疗6个月。
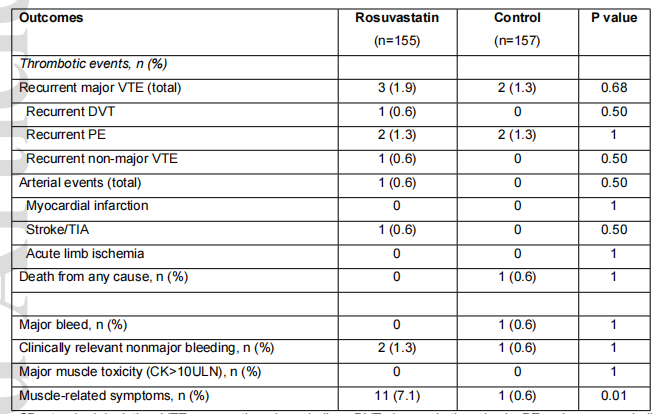
2016年11月至2019年12月期间,6个中心共有3391名患者进行了资格评估。在这些患者中,1347名(39.7%)患者符合条件并参与了试验,312名(23.1%)患者被随机分组。平均随机化率为每月8.2±4.3名患者。随访期间,研究人员观察到5例复发性VTE事件,瑞舒伐他汀组3例(1.9%)(2例肺栓塞,1例深静脉血栓形成)和对照组2例(1.3%)(2例肺栓塞)(p=0.68)。瑞舒伐他汀组发生1起大动脉事件,对照组未发生(0.6% vs. 0%,p=0.50)。
由此可见,该预试验的结果支持开展更大规模随机对照试验,以明确辅助瑞舒伐他汀对VTE二级预防的疗效。
原始出处:
Aurélien Delluc.et al.Statins for venous event reduction in patients with venous thromboembolism: a multicentre randomized controlled pilot trial assessing feasibility.Journal of Thrombosis and Haemostasis.2021.https://doi.org/10.1111/jth.15537
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#静脉血#
31
#他汀类药#
34
#静脉#
32
#HAE#
34
挺好
60
了解一下
68
学习学习
55