Cancer Treat Rev:免疫 pk 化疗,一线治疗晚期尿路上皮癌
2022-02-19 xiaozeng MedSci原创
无论是否耐受顺铂、无论PD-L1表达水平高低,晚期尿路上皮癌患者采用免疫抑制剂或化疗作为一线治疗的生存获益平分秋色
派姆单抗(Pembrolizumab)和阿替利珠单抗(Atezolizumab)已被批准用于一线治疗不适合以顺铂为基础的化疗且肿瘤高表达PD-L1的晚期尿路上皮癌 (aUC)。但是,这些免疫治疗药物的疗效与标准化疗相比孰优孰劣仍悬而未决,一直备受关注。
本研究目的是对比单药免疫肿瘤学 (IO) 化合物与铂类化疗在晚期尿路上皮癌中作为一线治疗的疗效。
研究人员系统地检索了从2016年1月至2021年5月期间PubMed、EMBASE、Web of Science 和 Scopus 数据库所收录的对比 IO 和化疗的3期临床试验。从已发表的 Kaplan-Meier 曲线中获取生存数据的算法用于重建总体生存 (OS) 数据。
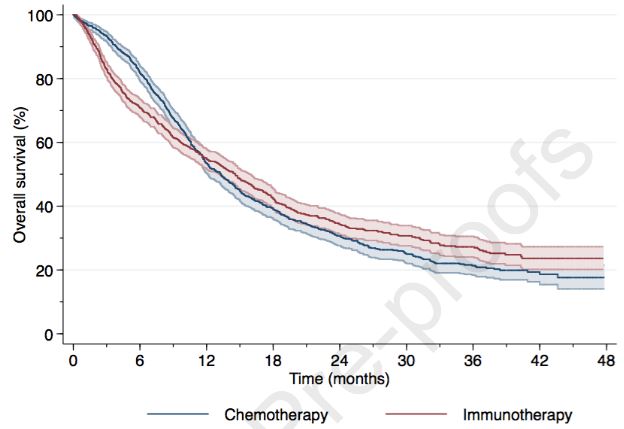
在总患者中,IO vs 化疗的总生存率
经筛选,最终纳入了3项对比 IO 和化疗的3期试验的2068位受试者。总体上,接受 IO(n=1013[49%])或化疗(n=1055[51%])治疗的患者的生存情况不相上下,24个月的受限平均生存事件差(ΔRMST)只有-0.4个月(p=0.2)。
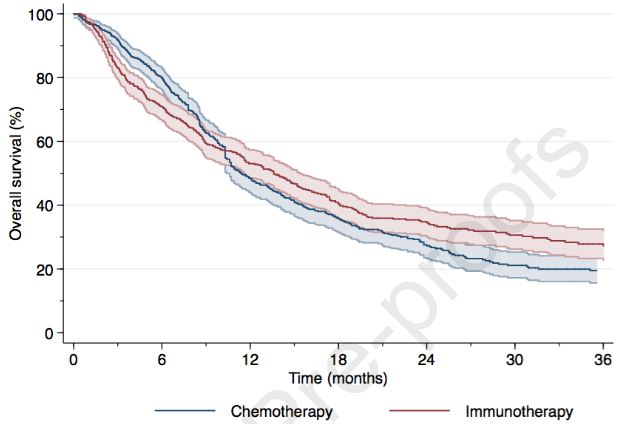
在顺铂不耐受患者中,IO vs 化疗的总生存率
不能采用顺铂治疗的患者采用 IO(n=509[49%])或其他药物化疗(n=530[51%])治疗的总生存情况也不分伯仲,24个月的ΔRMST只有0.1个月(p=0.7)。
在顺铂不耐受且高表达PD-L1的患者中,IO vs 化疗的总生存率
不适合顺铂治疗且高表达PD-L1的患者采用 IO(n=226[50%])或化疗(n=226[50%])治疗的总生存情况也无明显差异,24个月的ΔRMST为1.1个月(p=0.1)。
综上,该研究结果表明,无论是否耐受顺铂、无论PD-L1表达水平高低,晚期尿路上皮癌患者采用免疫抑制剂或化疗作为一线治疗的生存获益平分秋色。
原始出处:
Martini Alberto,Raggi Daniele,Fallara Giuseppe et al. Immunotherapy versus chemotherapy as first-line treatment for advanced urothelial cancer: A systematic review and meta-analysis.[J] .Cancer Treat Rev, 2022, 104: 102360.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#尿路上皮癌#
71
#TREAT#
53
#晚期尿路上皮癌#
42
#上皮癌#
37