Int J Urol:机器人辅助肾脏部分切除术在外生性、中生性和内生性肾肿瘤患者中的围手术期结果比较
2022-07-04 AlexYang MedSci原创
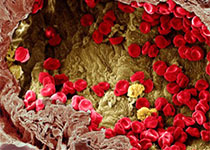
比较了接受机器人辅助肾脏部分切除术的外生性、中生性和内生性肾肿瘤患者的围手术期变量。
目前,PN被认为是局部小肾脏肿块患者的标准手术,因为与根治性肾切除术相比,PN能达到与之相当的肿瘤学效果,同时还能保持明显较好的肾功能。有资料显示,完全内生性肾肿瘤的肾部分切除术是一个极具挑战性的手术,即使在机器人手术系统的协助下,也存在一些技术上的困难。

近期,来自日本的研究人员在《Int J Urol》上发表文章,比较了接受机器人辅助肾脏部分切除术的外生性、中生性和内生性肾肿瘤患者的围手术期变量。

研究共纳入了265名接受机器人辅助肾脏部分切除术的局部小肾脏肿块患者。完全内生性肿瘤定义为完全被肾脏健康实质覆盖的肿块,根据术前计算机断层扫描的RENAL肾功能评分的'E'域得分,研究人员将受试者分为以下三组:外生性、中生性和内生性肿瘤组,并比较了这些组的围手术期结果。
在265名患者中,分别有127人、112人和26人分别归入外生型、中生型和内生型肿瘤组。内生性组的肿瘤直径明显小于其他组(P<0.001),而RENAL肾功能评分则明显较高(P<0.001)。此外,内生性肿瘤组的温热缺血时间明显长于其他组(P=0.009);然而,三组之间的三连胜结果没有明显差异。

手术和病理结果
综上所述,机器人辅助下的完全内生性肿瘤患者的肾脏部分切除术是一种可行的方法,不会明显损害围手术期的结果;然而,仍旧需要进一步调查这些患者的长期功能和肿瘤学结果。
原始出处:
Daisuke Motoyama, Toshiki Ito, Takayuki Sugiyama et al. Comparison of perioperative outcomes among patients with exophytic, mesophytic, and endophytic renal tumors undergoing robot-assisted partial nephrectomy. Int J Urol. Jun 2022
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#手术期#
41
#切除术#
39
#机器人#
51
#肾肿瘤#
34
#肿瘤患者#
39
#机器人辅助#
45
#机器#
40