Nat Commun:平滑肌中 AMPK 缺乏导致新生儿持续性肺动脉高压及过早死亡
2022-09-13 刘少飞 MedSci原创
越来越多的证据表明 AMPK 缺乏可能促进缺氧性和特发性肺动脉高压,其机制在很大程度上未知且治疗效果不佳。因此,重要的是要确定这个悖论的性质。
最近证实,AMP 活化蛋白激酶 (AMPK) 可促进缺氧性肺血管收缩 (HPV) ,这通过将血液从缺氧区域转移到富氧区域来帮助肺部的通气-灌注匹配,而且当疾病(例如慢性阻塞性肺病)和上升到海拔高度时,缺氧普遍存在时,会导致缺氧性肺动脉高压。与此形成鲜明对比的是,越来越多的证据表明 AMPK 缺乏可能促进缺氧性和特发性肺动脉高压,其机制在很大程度上未知且治疗效果不佳。因此,重要的是要确定这个悖论的性质。
AMPK 是一种细胞能量传感器,包含两个催化 α 亚基之一,以及两个 β 和三个 γ 调节亚基中的一个,它们共同提供至少 12 个异源三聚体亚基组合。AMP 与 γ 亚基的结合通过变构激活使 AMPK 活性增加 10 倍,AMP 或 ADP 的结合通过增加 α 亚基上 Thr172 的肝激酶 B1 (LKB1) 的磷酸化作用提供 100 倍的进一步活化,同时减少去磷酸化通过磷酸酶。这些效果中的每一个都被 ATP拮抗。还有三种 AMP 和 ADP 独立的 AMPK 激活途径:通过变构药物和代谢物 (ADAM) 位点调节长链脂肪酸; 通过果糖-1,6-二磷酸 (FBP) 传感机制调节葡萄糖,该机制可能涉及溶酶体上的醛缩酶-v- ATPase - Ragulator复合物;通过钙调蛋白活化激酶激酶 2 (CaMKK2) 进行的钙依赖性激活。一旦被激活,AMPK 的经典作用就是通过抑制合成代谢和激活分解代谢途径来维持细胞自主代谢稳态。AMPK 实现这一目标的部分原因是,它有助于控制自噬、线粒体生物发生和完整性以及线粒体氧化磷酸化和糖酵解之间的平衡。
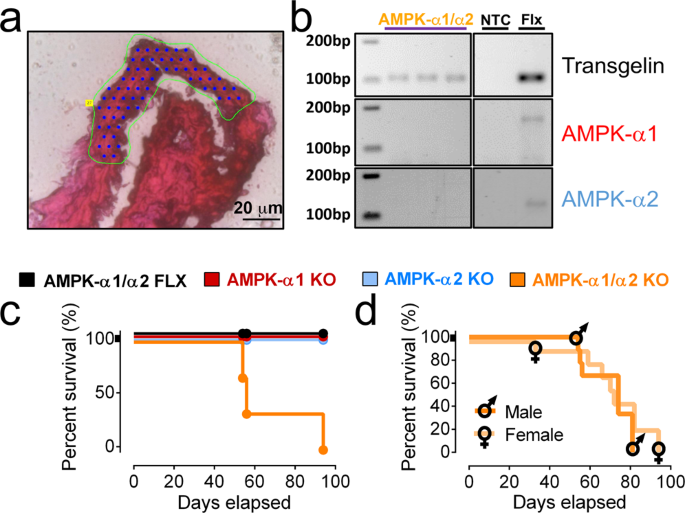
本研究揭示了平滑肌选择性 AMPK-α1/α2 缺乏与新生儿持续性肺动脉高压之间的直接联系。主要特征如下: (1) 整个肺动脉树的内侧厚度增加,并且在通常非肌肉的动脉中有明显的肌肉;(2)肺动脉肌细胞肥大而不是增殖;(3) 没有内膜纤维化、增生或丛状病变的证据(尽管丛状病变在小鼠模型中并不常见);(4)肺泡简化,肺泡数量减少,肺泡壁增厚,无肺泡内或间质水肿征象;(5) 肺血管阻力增加;(6)右心室扩张和右心室体积/重量比增加;(7) 右心室压力随年龄增加而心输出量减少;(8) 减少缺氧性肺血管收缩,从而导致急性缺氧性肺动脉高压;(9) 没有明显的实质纤维化或肺水肿,表明肺血管病变的出现独立于左心室功能障碍或慢性充血性心力衰竭。
参考文献:
Moral-Sanz J, Lewis SA, MacMillan S, Meloni M, McClafferty H, Viollet B, Foretz M, Del-Pozo J, Mark Evans A. AMPK deficiency in smooth muscles causes persistent pulmonary hypertension of the new-born and premature death. Nat Commun. 2022 Aug 26;13(1):5034. doi: 10.1038/s41467-022-32568-7. PMID: 36028487; PMCID: PMC9418192.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#平滑肌#
60
#Nat#
43
#COMMUN#
60
#动脉高压#
34
#过早死亡#
54