Cardiovasc Diabetol:普通人群糖化血红蛋白A1c水平与心血管结局的关系,全民HA1c筛查或成趋势!
2021-11-17 MedSci原创 MedSci原创
在非糖尿病参与者中,糖化血红蛋白水平升高与心血管疾病发病率和总死亡率相关,强调了糖化血红蛋白水平在整个人群中的重要性。
评估普通人群的心血管风险对临床决策很重要,尽管临床已经发现了很多新的独立的生物标志物,但心血管风险的评估依然依赖于一组传统的心血管风险因素(CVRFs),如年龄、性别、血压、血脂水平、糖尿病(DM)和吸烟等。是否在心血管风险评估中纳入新的生物标记仍然是一个值得争论和研究的话题。
糖尿病被认为是心血管疾病(CVD)的经典危险因素。为了改善心血管风险评估及探索新的危险因素,糖化血红蛋白或血红蛋白A1c (HbA1c)可能是一个潜在的候选者,在普通人群中,其与心血管结果的关联强度仍不确定。本研究旨在评估普通人群中糖化血红蛋白与心血管结局的相关性。
研究者对来自欧洲的6项前瞻性人群队列研究的数据进行了分析,其中包括36180名参与者。在无糖尿病(N=32496)和糖尿病(N=3684)的受试者中,结合经典心血管风险因素(CVRFs)评估HbA1c与心血管死亡率、心血管疾病(CVD)发病率和总死亡率的相关性。
Kaplan-Meier曲线显示随着HbA1c水平的升高,心血管事件发生率更高。Cox回归分析显示总研究人群中HbA1c(单位:mmol/mol)与检查结果之间存在显著相关性。因此,HbA1c每增加10 mmol/mol,心血管死亡率的危险比(HR)为1.16,CVD发病率为1.13,总死亡率为1.09。
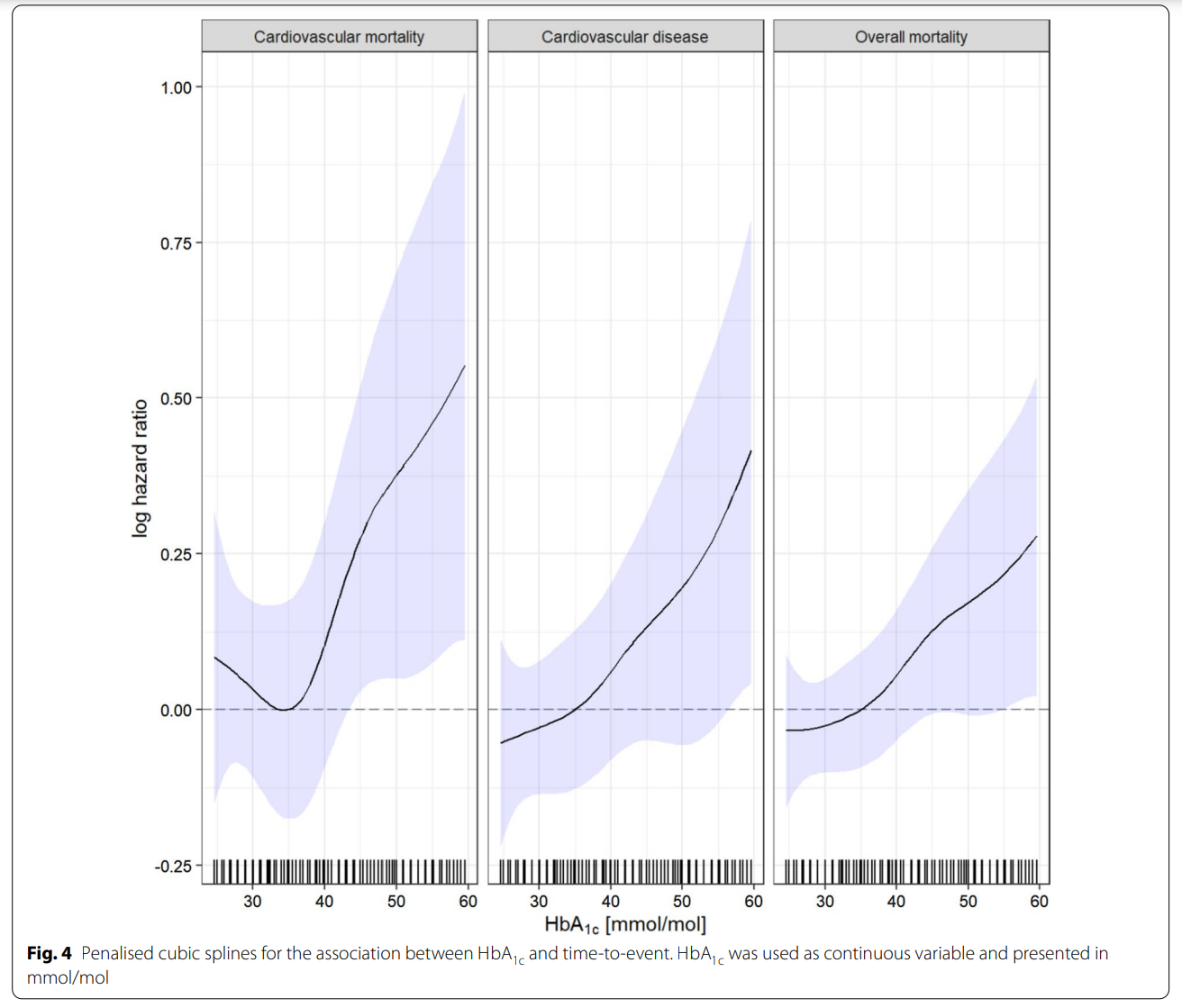
HbA1c与事件发生时间之间关联的三次样条
在无糖尿病且HbA1c水平升高的研究参与者中,也观察到与CVD发病率和总死亡率的相关性。心血管死亡率、心血管疾病发病率和总死亡率的HbA1c临界值分别为39.9 mmol/mol(5.8%)、36.6 mmol/mol(5.5%)和38.8 mmol/mol(5.7%),也显示风险增加。
总之,本研究显示糖化血红蛋白与欧洲普通人群的心血管死亡率、总死亡率和心血管疾病独立相关。糖化血红蛋白水平与预后之间的关系基本呈单调递增关系。在非糖尿病参与者中,糖化血红蛋白水平升高与心血管疾病发病率和总死亡率相关,强调了糖化血红蛋白水平在整个人群中监测的重要性。
参考文献:Sinning, C., Makarova, N., Völzke, H. et al. Association of glycated hemoglobin A1c levels with cardiovascular outcomes in the general population: results from the BiomarCaRE (Biomarker for Cardiovascular Risk Assessment in Europe) consortium. Cardiovasc Diabetol 20, 223 (2021). https://doi.org/10.1186/s12933-021-01413-4
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#ASC#
24
#BET#
24
#DIA#
34
#血红蛋白A1c#
34
#心血管结局#
0
#普通人群#
28