Canakinumab可将痛风发生率降低一半以上
2018-06-24 MedSci MedSci原创
痛风是一种非常常见的疾病,是一种由于嘌呤生物合成代谢增加,尿酸产生过多或因尿酸排泄不良而致血中尿酸升高,尿酸盐结晶沉积在关节滑膜、滑囊、软骨及其他组织中引起的反复发作性炎性疾病
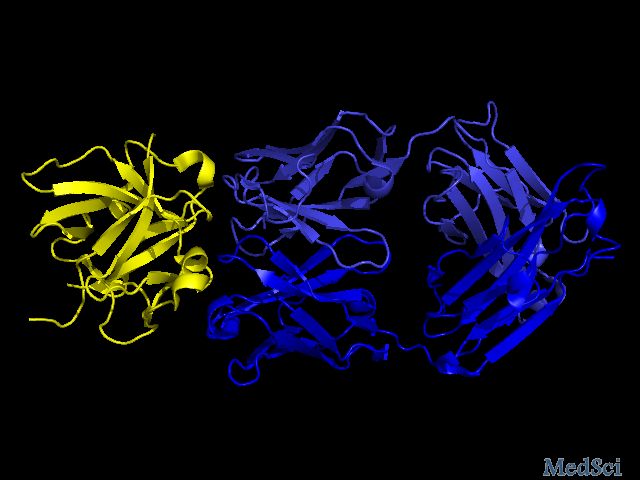
痛风是一种非常常见的疾病,是一种由于嘌呤生物合成代谢增加,尿酸产生过多或因尿酸排泄不良而致血中尿酸升高,尿酸盐结晶沉积在关节滑膜、滑囊、软骨及其他组织中引起的反复发作性炎性疾病。它是由于单钠尿酸盐结晶(MSU)或尿酸在细胞外液形成超饱和状态,使其晶体在组织中沉积而造成的一组异源性疾病。通风会在几个小时内发展并在关节中引起剧烈的疼痛,其临床特征为:高尿酸血症及尿酸盐结晶、沉积所致的特征性急性关节炎、痛风石、间质性肾炎等。Canakinumab是一种单克隆抗体,可阻断由白细胞介素-1β介导的炎症途径。它被授权用于治疗一些罕见的自身炎症疾病,但也可用于治疗某些患有标准治疗禁忌症的痛风患者。
在欧洲风湿病学年会(EULAR 2018)上发表的一项研究结果表明,与安慰剂相比,canakinumab可显著降低痛风发生率,而无论基线血清尿酸水平如何。EULAR科学计划委员会主席RobertLandewé教授在评论这项研究结果时说:“这些都是显著的结果,证明了canakinumab在痛风患者中的潜在预防作用。这项研究也将有助于我们了解痛风、尿酸和心血管疾病之间的相互作用”。
原始出处:
https://www.europeanpharmaceuticalreview.com/news/76480/canakinumab-reduces-gout-rate/
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#mAb#
33
#发生率#
33
#ANA#
29
#AKI#
25
#Canakinumab#
32