Bone Research:面对超加工食品,少吃也是徒劳!
2021-04-20 MedSci原创 MedSci原创
超加工食品是在已经加工过的食品基础上再加工的食品,这类食品通常含有五种以上工业制剂,并且是高糖、高脂、高热量的食品。
超加工食品是在已经加工过的食品基础上再加工的食品,这类食品通常含有五种以上工业制剂,并且是高糖、高脂、高热量的食品。大量研究显示,超加工食品对机体产生负面影响。然而很少有研究关注其对儿童,特别是在幼儿成长中骨骼发育的影响。

近日,发表在Bone Research杂志的一项研究显示,超加工食品对骨骼发育产生重大影响。成年大鼠中食用仅由超加工食品组成的饮食可导致胫骨生长板发生重大改变。同时,小梁和皮质骨的质量显着下降,致密骨中孔隙分布广泛,所有这些都与纵向生长的延迟和骨脆性有关。

食用超加工饮食会导致生长迟缓,并导致骨骼结构和生物力学特性的改变.
具体而言,经过组织学检查,研究人员发现,喂食富含脂肪和糖的超加工食品的大鼠的胫骨生长板发生病变,导致发育迟缓。同时,骨密度显著降低,并且骨的结构参数发生恶化,在皮质中呈现出筛状外观,而在长骨和椎骨中呈现出差的小梁参数。这导致整个骨骼的机械性能较差,骨折风险很高。
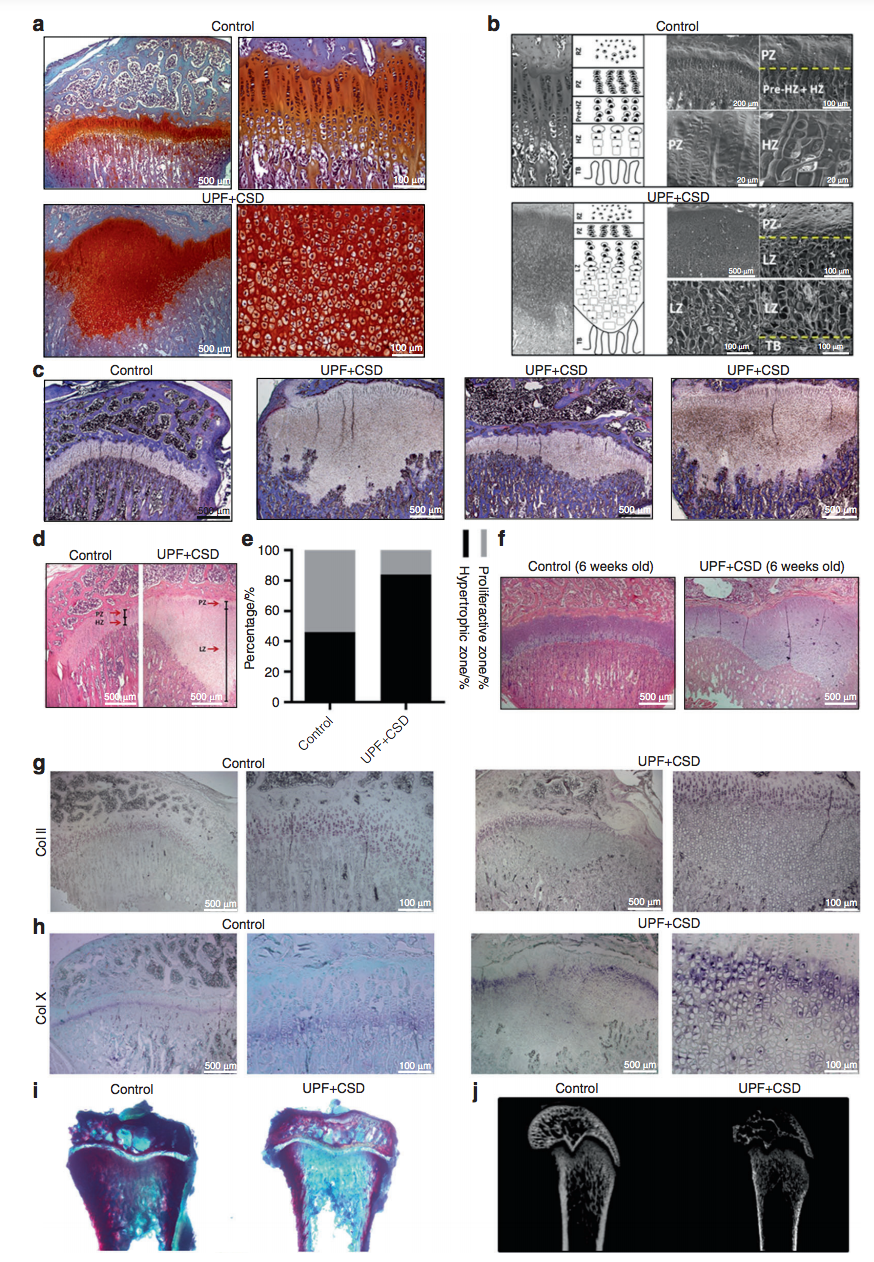
食用超加工饮食会导致生长板受损,软骨细胞分化过程改变.
研究人员进一步分析了特定的饮食习惯对骨骼发育的影响,将大鼠每周的食物摄人划分为30%来自’控制’食物,70%来自超加工食物。研究发现,大鼠的骨密度受到了中等程度的损害,尽管在其生长板中很少出现软骨积聚的迹象。对此,研究人员表示,即使减少超加工食品的摄入量,也可能对骨骼生长产生一定的负面影响。
研究人员表示,这些发现至关重要,因为近几十年来,食品供应一直以加工量大,即食产品为主。本质上,世界上所销售的75%的食品为加工食品。在过去的30年里,婴幼儿对超加工食品的摄入明显增加,50%的美国儿童每天都吃这些食品。即使我们减少脂肪以及其他有害物质的摄入,这些食品仍然具有其破坏性。已有众多证据表明,人体的每个部位都容易受到这种损害,当然,那些处于发展关键阶段的系统也很容易受到损害。”
综上,这项研究首次发现,食用超加工食品对骨骼生长的严重影响。这种病理学的改变远远超出了已知的代谢作用所解释的范围,因此,骨骼健康或成为现代饮食研究的新目标。
原始出处
Janna Zaretsky et al. Ultra-processed food targets bone quality via endochondral ossification, Bone Research (2021). DOI: 10.1038/s41413-020-00127-9
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Bone#
39
不吃太难了
66
#Research#
38
少吃不如不吃
77
好文章
63