British Journal of Sports Medicine:保持“金鸡独立”的时长,与你未来7年的死亡风险息息相关
2022-07-12 文竞择 生物探索
由于平衡的实现需要靠视觉感知、肌肉力量、神经系统等多重机制相互协调,平衡力出现问题,往往反映出身体的系统性障碍。有研究表明,单腿站立时长与未来7年死亡风险密切相关。
导语:平衡是人们日常生活和体育活动中必须具备的一种能力。站、坐、蹲、骑等姿势都离不开平衡能力。由于平衡的实现需要靠视觉感知、肌肉力量、神经系统等多重机制相互协调,平衡力出现问题,往往反映出身体的系统性障碍。近期,有一项研究表明,单腿站立时长与未来7年死亡风险密切相关。下面,让我们来一探究竟。
2022年6月21日,巴西运动医学诊所、东芬兰大学、悉尼大学、布里斯托大学和斯坦福大学的研究团队在British Journal of Sports Medicine发表题为“Successful 10-second one-legged stance performance predicts survival in middle-aged and older individuals”的研究成果(图1)。研究发现中年和老年参与者无法完成10秒单腿站立(One-legged stance,OLS)与更高的全因死亡率风险相关,与更短的预期寿命有关。
图1 研究成果(图源)
全球每年约有70万人死于跌倒,其中80%以上在低收入/中等收入国家,跌倒也是全球因意外伤害导致死亡的第二大原因。平衡能力与许多日常生活活动相关,大量证据表明,平衡障碍对健康有害,但一些运动干预可能会改善平衡。然而,平衡评估并未纳入中老年人的常规临床检查中,这可能部分归因于平衡测试的标准化程度低,以及与有氧健身等情况相比,平衡状况与跌倒造成的临床结果(例如死亡率)相关的数据相对缺乏。在这种情况下,简单、廉价、可靠和安全的平衡评估工具可以帮助预测中老年人生存率,这可能对评估和治疗老年人的卫生专业人员有所助益。
此项研究为前瞻性队列研究,使用来自CLINIMEX运动队列数据。CLINIMEX运动队列研究成立于1994年,旨在评估各种身体健康指标和其他运动相关变量以及常规心血管危险因素与全因和特定原因死亡率结果之间的关系。研究人员对2008年至2020年间,1702名51-75岁的个体(68%为男性)进行人体测量、临床和生命状态以及10秒OLS数据进行评估(图2)。评估完成10秒OLS测试的能力是否与中老年男性的全因死亡率独立相关,以及10秒OLS是否在普通人口统计、人体测量和临床数据之外添加了相关的预后信息。
图2 10秒单腿站姿测试的身体姿势(图源)
研究结果表明:
1. 在随后7年内,无法完成10秒OLS的参与者死亡率比可完成组高12.9%
在1702人中,共有348名(20.4%)参与者未能通过10秒OLS测试,被标记为NO,其他完成的参与者被标记为YES。在随后7(4.16–9.41)年的中位随访时间中,123名参与者(7.2%)死亡,死因主要为癌症(32%)、心血管疾病(30%)、呼吸系统疾病(9%)和COVID-19并发症(7%),死亡没有明显的时间趋势(P=0.77)。在1702人的样本中,有123起全因死亡事件,我们有92%的能力检测到临床上重要的风险比(Hazard Ratio,HR)为1.84。NO组的死亡比例高于YES组(17.5% vs 4.6%;P<0.001),反映绝对差异为12.9%,但主要潜在死因分布无显着差异(P=0.45)。
2. 无法完成10秒OLS的参与者无性别差异,但健康状况普遍较差
虽然性别分布在YES和NO组之间没有显着差异(P=0.76),但其他几个变量,包括年龄、BMI(Body Mass Index)和腰高比在两组之间存在差异(P<0.001);除身高外,NO组与所有其他变量显着相关(P <0.001);NO组和所选连续变量之间的两个最高相关系数是年龄(0.40)和腰高比(0.26);一般来说,NO组参与者的健康状况较差,患有冠状动脉疾病、高血压、血脂异常和肥胖的参与者比例较高;两组最显着的差异是糖尿病发病率,NO组(37.9%)约为YES组(12.6%)的三倍(P <0.001)(图3)。
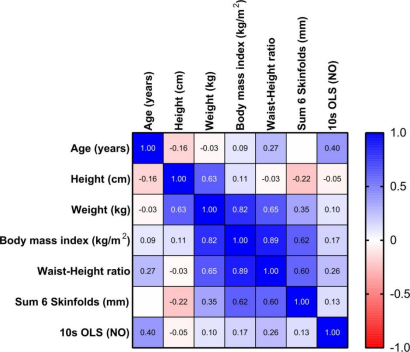
图3 NO组与人口统计学和人体测量学变量之间的Spearman相关系数(图源)
3. 无法完成10秒OLS的参与者与更高的全因死亡率相关
YES和NO组的Kaplan-Meier生存曲线显着不同(P<0.001);Cox比例风险分析表明,NO组与显着更高的全因死亡率风险相关;多变量(年龄、性别、BMI和临床合并症(包括冠状动脉疾病史、高血压、糖尿病、肥胖和血脂异常))调整结果显示YES和NO组HR(95% CI)分别为2.18(1.48至3.22;p<0.001)和1.84(1.23至2.78;p=0.003);将NO组添加到包含已确定风险因素的模型中,与通过-2对数似然的差异和综合鉴别改进的差异来衡量的死亡风险,发现结果得到显着改善。
此项研究表明,中年和老年参与者无法完成10秒OLS,与随后七年内更高的全因死亡率风险相关,与更短的预期寿命有关。此项研究的优势在于10秒OLS测试是在卫生专业人员的直接监督下进行的;10秒OLS测试很容易向参与者解释、应用并获得研究中使用的二元结果(是或否响应者);中位随访时间和样本中的死亡百分比为分析和解决研究目的提供了适当的统计能力;此外,还有可用于临床相关多变量建模的几个人体测量学和临床变量的数据。
此项研究存在一定局限性。首先,CLINIMEX队列主要由白人参与者组成,属于巴西较高的社会经济阶层,应谨慎将这些发现类推到与此概况不同的人群;可能存在更复杂的OLS平衡测量,以更好的区分并提高在预测生存率方面的价值。然而,这将使平衡测试变得更加复杂,更难被纳入临床常规实践;其次,HR难以解释风险因素之间的差异,还意味着在整个随访过程中始终存在相对危险;此外,由于对幸存者进行了筛选,具有内置的选择;无法获得几个潜在的混杂变量,包括近期跌倒史、体育活动或锻炼模式以及运动习惯、饮食、吸烟和使用可能干扰平衡的药物;由于没有重复测量暴露,本研究无法解决受先前暴露影响的时变混杂因素,并提供纠正潜在回归稀释偏差的机会;由于研究的样本量相对有限,本研究没有使用K折交叉验证的方法;最后,需要研究可能解释观察到的OLS平衡不良与全因死亡率之间关联的生物学机制;研究更详细或更复杂的静态平衡评估指标(例如包括压力位移中心的测量、所需试验次数、不同的手臂或足部位置、在OLS期间闭眼)是否也有助于生存分析。
原始出处:
Araujo CG, de Souza E Silva CG, Laukkanen JA, et al. Successful 10-second one-legged stance performance predicts survival in middle-aged and older individuals. Br J Sports Med. 2022 Jun 21:bjsports-2021-105360. doi: 10.1136/bjsports-2021-105360. Epub ahead of print. PMID: 35728834.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#CIN#
55
#DIC#
40
#死亡风险#
44
#Medicine#
38
#Med#
36
非常实用
44
学习
50